William G. Nelson, MD, PhD Photo by Joe Rubino
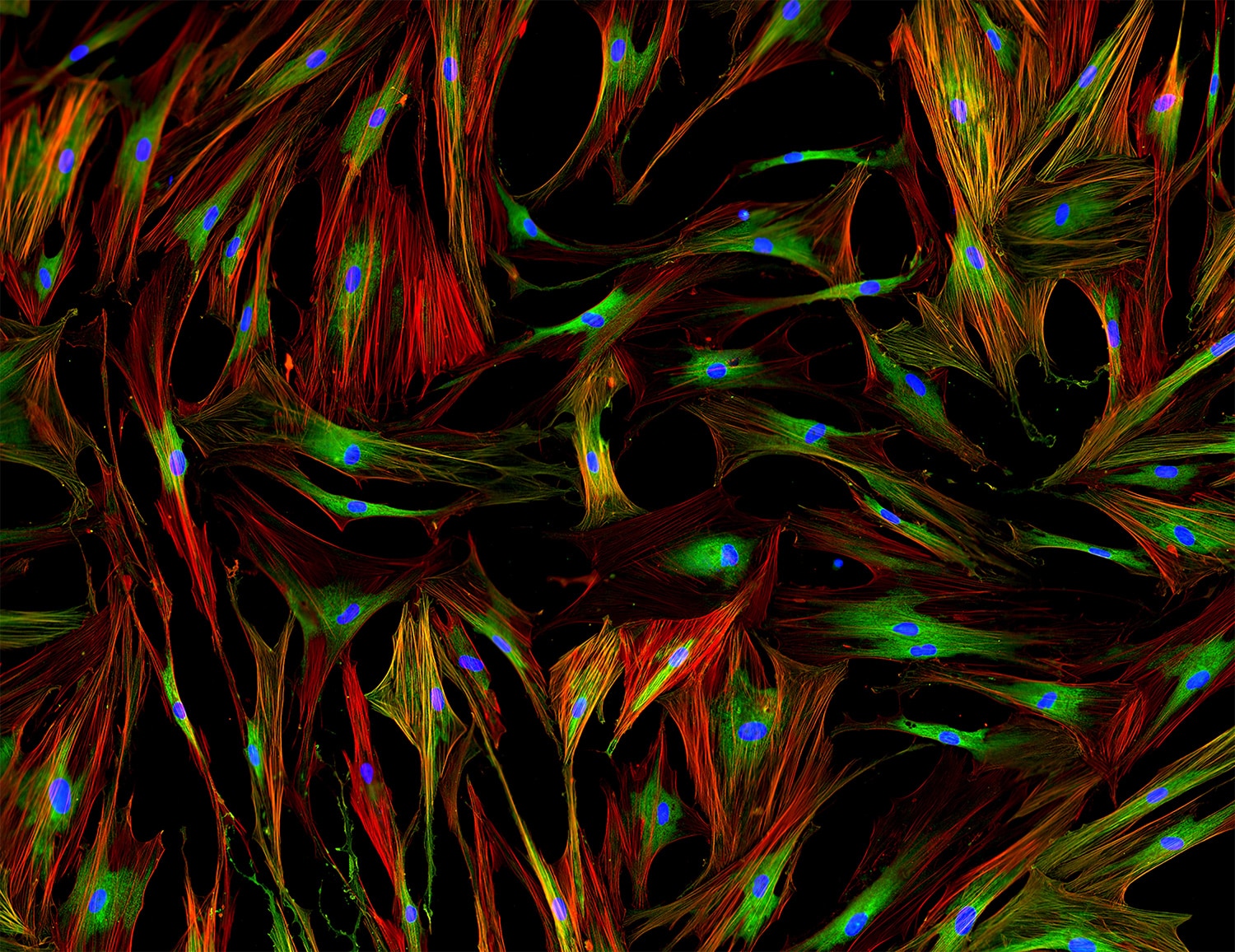
CANCERS THAT GROW and disseminate to threaten life reside amid many types of noncancerous cells, including blood vessel cells, supportive cells called fibroblasts, and immune cells. These cells comprise the tumor microenvironment, an ecosystem that helps cancer cells evade destruction by the immune system, avoid death caused by anti-cancer drugs, and exhibit ever more malignant behaviors. As researchers identify and characterize the components of this cancer ecosystem, new opportunities are emerging to build better treatments.
Left unchecked, cancer cells tend to increase their numbers uncontrollably and outstrip their blood supply. Starved for oxygen and nutrients, cancer cells survive by stimulating new blood vessel growth. One of the signals used by cancer cells to respond to oxygen deficiency, also known as hypoxia, is the activation of hypoxia-inducible factor 1-alpha (HIF-1-alpha), a mechanism elucidated by the researchers Gregg L. Semenza, William G. Kaelin and Peter J. Ratcliffe. Their discoveries earned the three men the 2019 Nobel Prize in Physiology or Medicine. HIF-1-alpha directs the production and release of vascular endothelial growth factor (VEGF), the principal stimulator of new blood vessel cell growth. In 2004, Avastin (bevacizumab), the first of many agents that block VEGF-stimulated blood vessel growth, was approved by the Food and Drug Administration to treat cancer by targeting the tumor microenvironment.
Fibroblasts are cells that form the connective tissues in the body, producing structural molecules for each of the organs and contributing to wound healing and repair. Cancer cells co-opt fibroblasts to assist in new blood vessel recruitment, remodeling tissue structure and holding immune cells at bay. A series of studies authored by Ashani Weeraratna and her colleagues have hinted that aging skin fibroblasts may be more likely to promote melanoma cell dissemination than younger fibroblasts, a finding that may explain why melanoma appears more likely to threaten life in older adults. Drugs aimed at cancer-associated fibroblasts are working their way through human clinical trials for many different cancers.
Immune cells otherwise capable of recognizing and destroying cancer cells fail to do so in the tumor microenvironment. There are likely many ways in which the immune responses are held in check. For some cancers, like many melanomas and lung cancers, T cells can be unleashed to kill cancer cells upon administration of immune checkpoint inhibitors such as Yervoy (ipilimumab), Opdivo (nivolumab) and Keytruda (pembrolizumab). When successful, responses to these treatments can be spectacular. Unfortunately, immune checkpoint inhibitors are not as effective in treating breast, prostate and pancreatic cancers.
One challenge to effective treatment may be that cancer cells, as residents of the tumor microenvironment, are aggressive consumers of nutrients and relentless polluters. To propagate quickly, cancer cells need to duplicate themselves, voraciously consuming the limited supply of oxygen and other nutrients and restricting the amounts of oxygen and nutrients available to immune cells and other cells in the microenvironment. In addition, the growing mass of cancer cells produces a prodigious amount of waste materials like lactic acid, which further weakens immune cell functions.
These mechanisms may create an opportunity for new drugs that selectively interfere with metabolism in cancer cells. Along with glucose, cancer cells take up amino acids like glutamine to fuel their dysregulated growth. Early preclinical studies of a prodrug—an inert compound metabolized into an active drug once it enters the body—that blocks glutamine metabolism in the tumor microenvironment hint that cancer cell growth can be slowed while simultaneously allowing improved anti-cancer immunity. If these drugs can curb cancer cell gluttony and reduce waste, the tumor microenvironment could be rendered hostile to cancer cells, making them vulnerable to being treated with more traditional anti-cancer drugs.
Cancer cells that proliferate relentlessly, invade healthy organs and tissues, and metastasize to distant sites in the body rely heavily on the support system they create. As cancer researchers learn more about the microenvironment surrounding cancer cells, future cancer treatments may target both cancer cells and their corrupted ecosystems.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.