NEW TREATMENTS such as immune checkpoint inhibitors and targeted therapies have delivered durable and long-term responses in patients with metastatic melanoma. But almost half of people with metastatic melanoma will die from the disease within five years.
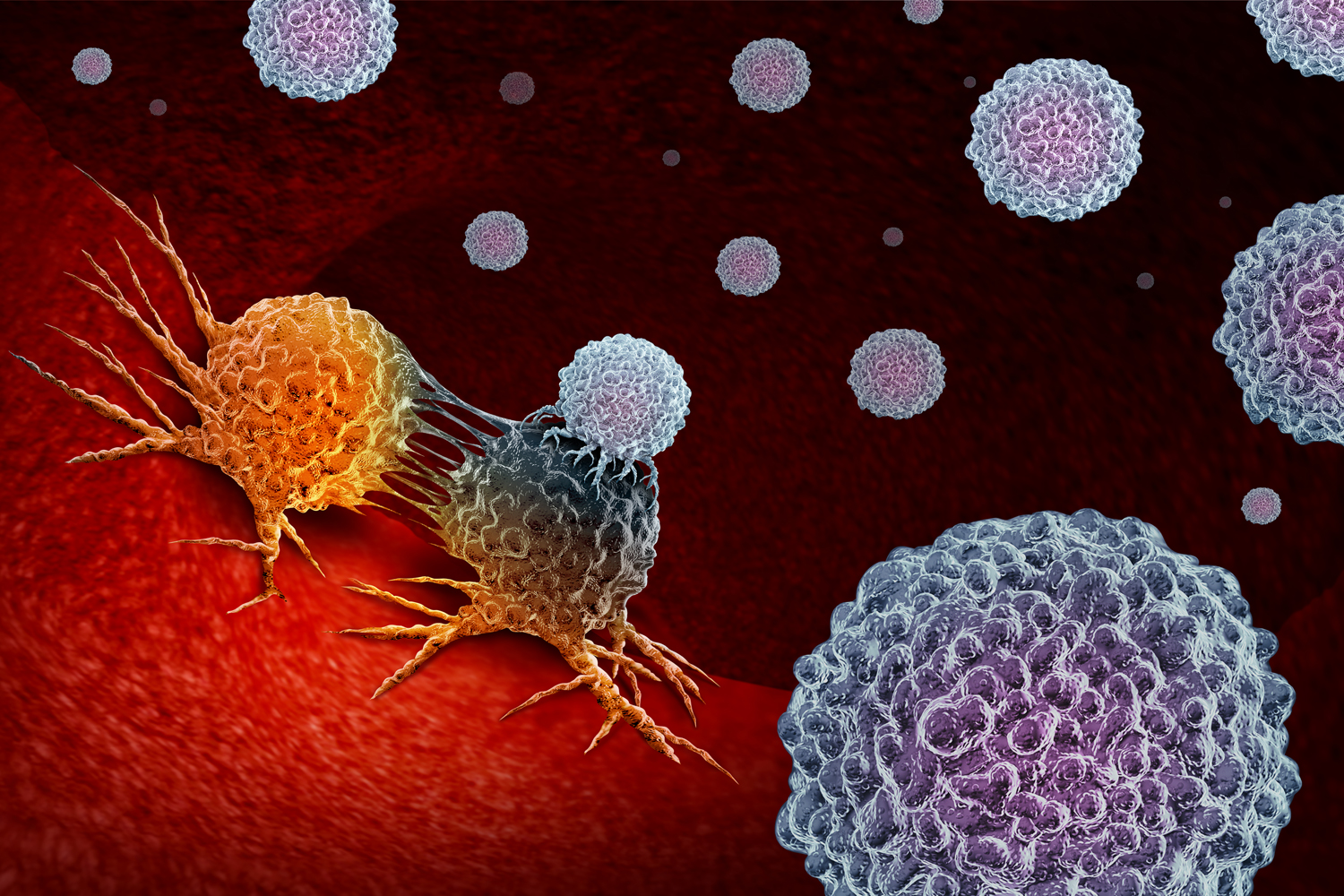
A type of adoptive T-cell therapy, called tumor-infiltrating lymphocyte therapy, may provide another option for people whose melanoma has advanced after multiple rounds of treatment. This experimental treatment involves harvesting T cells from a patient’s tumor tissue. The extracted T cells, called tumor-infiltrating lymphocytes (TILs), are exposed to an agent called interleukin-2, which promotes their growth over a few weeks. After this expansion, the TILs are infused back into the patient’s body, where they attack the cancer.
A study published Dec. 8, 2022, in the New England Journal of Medicine divided patients with metastatic melanoma into two groups that would receive either TIL therapy or a type of immune checkpoint inhibitor called Yervoy (ipilimumab). Overall, 19 patients in the study had no prior treatment for metastatic melanoma, while the remaining 149 patients had previous treatments, including anti-PD-1 therapies, a type of immune checkpoint inhibitor used to treat melanoma.
Patients in the group that received TILs had a median progression-free survival of 7.2 months, compared with 3.1 months in the group that received Yervoy. The median overall survival was 25.8 months in the TIL group and 18.9 months in the Yervoy group. Of note, 17 patients who received TILs had a complete response, meaning their tumors went away, compared with six patients in the group that received Yervoy.
“TIL [therapy] has been shown to result in responses even when immune checkpoint inhibitors do not work,” says John B.A.G. Haanen, a medical oncologist and group leader for the Netherlands Cancer Institute who is the principal investigator for the study.
Prior to TIL infusion, patients receive chemotherapy to deplete the body of immunosuppressive cells. After the infusion, patients also receive high-dose interleukin-2, which stimulates growth of the TILs. “[TIL therapy] is given largely in the hospital and is certainly not a walk in the park. Side effects come from the chemotherapy and the interleukin-2 but are transient,” with almost all patients making a full recovery after a few weeks, Haanen says.
In March 2023, biopharmaceutical company Iovance submitted an application for its TIL therapy to the Food and Drug Administration. Approval would clear the way for the therapy to be available for treating metastatic or unresectable melanoma that has progressed after other treatments have stopped working.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.