Cancer affects every one of us in some way, but I didn’t expect to be one of those who receive the diagnosis. In 2017, I had an ultrasound after my primary care doctor felt a lump in my throat during a routine physical. The lump ended up being benign, but the test also detected a tumor that turned out to be stage I papillary thyroid cancer. I was 27 years old.
I was lucky. Symptoms of thyroid cancer can include a lump or swelling in the neck as well as trouble swallowing and breathing. But I didn’t have any symptoms going into my diagnosis and very few during my treatment.
What I did hear repeatedly from various physicians was that I had the “good cancer,” and that “if you were to have a cancer, thyroid would be the one to get.”
I took the comments into consideration. However, I quickly learned that there is no such thing as a good cancer, and I believe that medical professionals should stop saying certain cancers are good.
The following are facts about thyroid cancer I have learned since my diagnosis.
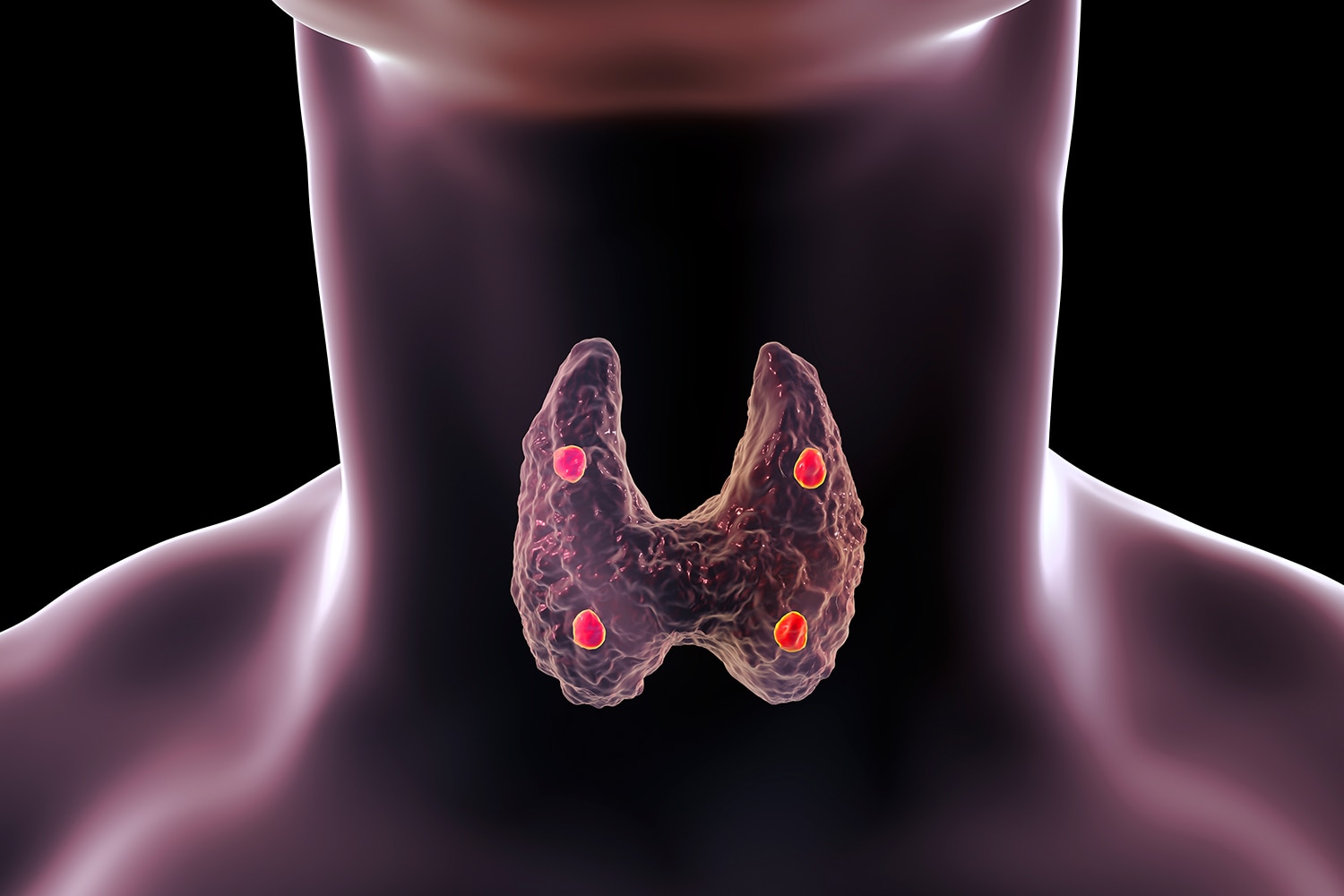
Different types of thyroid cancer have different levels of severity. I was diagnosed with the most common type of thyroid cancer, called papillary thyroid cancer, accounting for more than 80% of all cases. The other four types include follicular (10%), Hürthle cell (3%), medullary (4%) and anaplastic (2%). Papillary thyroid cancer is the least aggressive and is slow growing. Follicular thyroid cancer also comes with a relatively good prognosis. The rarer types of thyroid cancer are harder to treat.
There are various stages of thyroid cancer. Within types, thyroid cancer can be classified by stages ranging from I to IV. Stages explain how severe the cancer is, as well as how much of it is in the body, based on tumor size, nearby spread to lymph nodes, and metastases to different sites. Thyroid cancer is unique in its staging compared to other types of cancer, however, in that it takes the patient’s age into account. Patients who are diagnosed at a younger age tend to have a better prognosis and will be staged lower than older patients with the same extent of cancer. For example, a patient with papillary or follicular thyroid cancer that has spread to distant parts of the body who is age 55 or older has stage IVB or IVC cancer, but a patient with distant metastasis who is under 55 is said to have stage II thyroid cancer.
My cancer had spread to nearby lymph nodes. However, because thyroid cancer has a very low mortality rate and I was under age 55, my cancer was classified as stage I. The cancer in the lymph nodes had not been identified during the ultrasound that found my tumor, so I underwent a partial thyroidectomy to salvage the thyroid as much as possible. However, when the lymph nodes tested positive for cancer during the surgery, I was required to undergo a second surgery a few months later to remove the other half of the thyroid. I also underwent radioactive iodine therapy, which is radiation that kills any remaining thyroid cells, including cancerous ones. Learning this, I wondered how the cancer in the lymph nodes had not been detected earlier. Why was this happening to me, and what did I do to deserve this? While the news was a little confusing and heartbreaking to understand at first, I was appreciative to learn about my prognosis.
Thyroid cancer treatment can have long-lasting effects. After treatment is completed, patients must still have regular appointments with an endocrinologist or oncologist. The thyroid secretes hormones that help regulate metabolism and other essential bodily functions. Following a total thyroidectomy, patients must take thyroid hormone for the rest of their lives. It can take a while for a physician to pinpoint the right dose. During this process, a patient can experience symptoms of hypothyroidism (too small of a dose), including fatigue, weight gain, elevated cholesterol and slowed heart rate. Other patients experience symptoms of hyperthyroidism (too large of a dose), including tremors, anxiety, irritability, heart palpitations and difficulty sleeping. Thyroid cancer and its treatment can also affect mental health. Anxiety, nervousness, depression, fatigue and guilt can all accompany a diagnosis.
Other people are there for you. Going through a cancer journey is hard, and I’ve learned that you can’t do it alone. Having caregivers, friends and family for both emotional and physical support can help immensely. Even though they don’t know exactly what you’re going through, I have found that having someone to talk to can help reduce stress.
Additionally, joining a support group at any stage of the journey, from diagnosis to end of treatment and into survivorship, can answer the longing to know you’re not the only one facing the challenge. For example, public and private groups on Facebook, such as Papillary Thyroid Cancer Support, are formed by hundreds or sometimes thousands of people interested in discussing a specific type of cancer, such as thyroid cancer, or even a specific cancer subtype, such as papillary thyroid cancer.
Outside the online community, you can find support groups through local hospitals, the American Cancer Society resource search tool or a quick Google search. Knowing there are other people like me who are experiencing the same thing and being able to share my feelings and emotions in a judgment-free zone has fueled me with strength I will need for the rest of my life. While I had to join the club that no one ever wants to join, I am proud to call myself a survivor and advocate for other patients.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.