BLOOD CLOTS are a leading cause of death in people with cancer, second only to cancer itself. People with cancer have nine times the clotting risk of people without cancer.
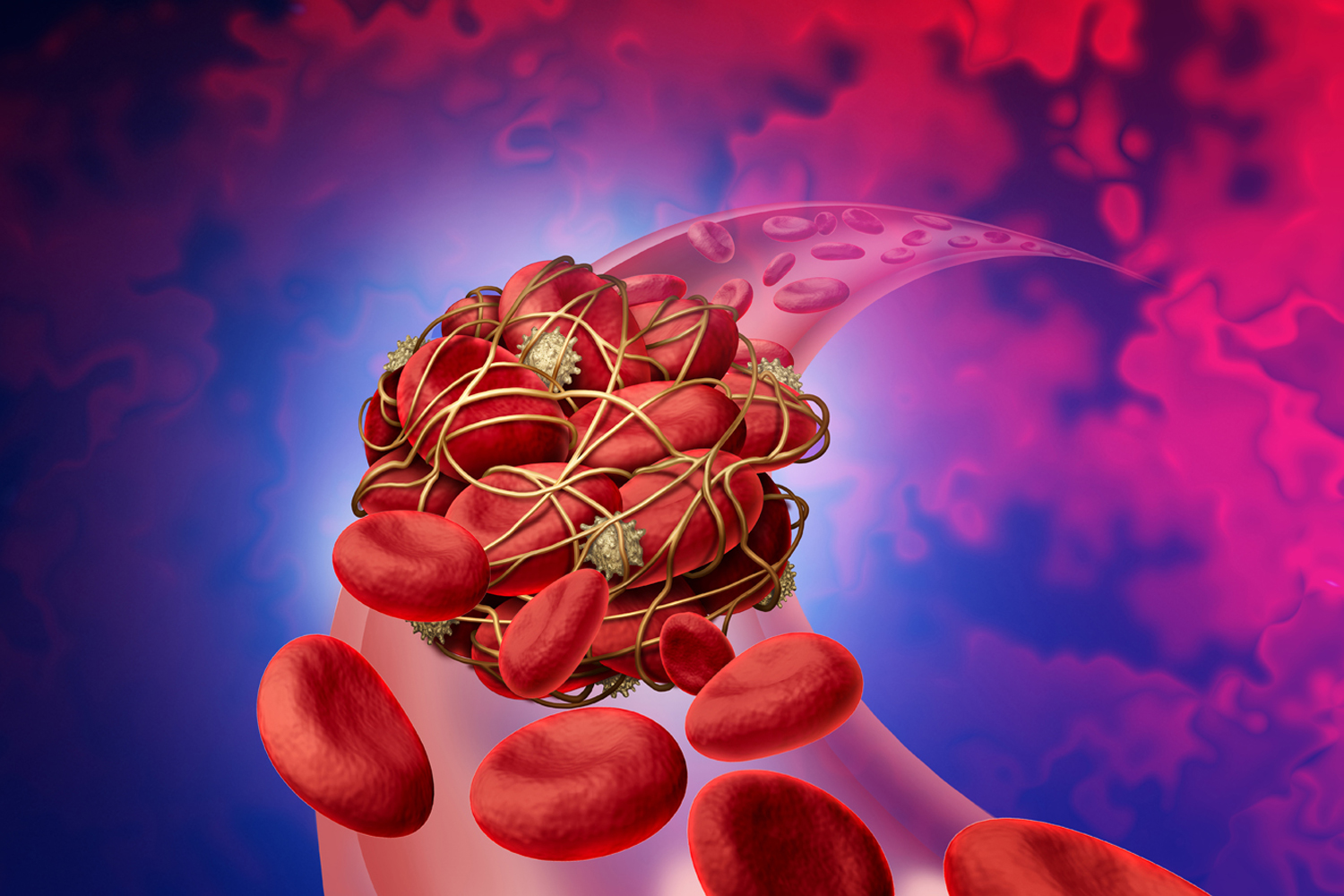
Blood clots can serve an essential function: to stop bleeding. When blood clots form inside blood vessels in the absence of bleeding, however, they can block blood flow. These dangerous blood clots usually form in veins and are called thrombi. A common example of this is deep vein thrombosis (DVT), which occurs when a clot forms in one of the deep veins of the body, often in the leg.
If a clot breaks free of the vein, it can travel to the heart and block an artery bringing deoxygenated blood to the lungs. This is called a pulmonary embolism, and it can be life-threatening.
To increase awareness of the clotting risk that cancer patients face, the National Comprehensive Cancer Network (NCCN) released patient guidelines in August 2023, based on the organization’s clinical guidance for oncologists. Cancer Today spoke with Michael B. Streiff, a medical oncologist from Johns Hopkins Medicine in Baltimore who chaired the NCCN clinical guidelines committee, about how people with cancer can reduce their clotting risk.
CT: Why are cancer patients at elevated risk for blood clots?
STREIFF: Cancers grow by getting access to blood vessels and oxygenated blood. They put people at risk for blood clots because the chemicals they release stimulate the clotting cascade.
And a side effect of cancer treatments also tends to be clot formation. That applies to all the different therapies we use, from chemotherapy to immunotherapy to targeted therapies. Some treatments damage blood vessels. Dead cells tend to promote clot formation. Surgery increases risk of clots because when you’re cutting [tumors] out, you need the clotting system activated where you’re doing your cutting, but at the same time, that clotting activation is systemic. Afterwards, people are often not moving around. You’re in a bed, you’re taking a while to recover. All that puts you at risk for having a blood clot.
CT: What are the key strategies for preventing blood clots?
STREIFF: Blood thinners, which block one or more of the proteins that are involved in forming clots, are one way we prevent blood clots.
The other way is using devices that result in blood circulation. There are boot-like garments that squeeze the legs to pump the blood back towards your heart. By doing that, they’re re-creating ambulation, or walking around, and that’s how they decrease blood clots.
CT: What can patients do on their own to reduce their risk of blood clots?
STREIFF: In general, a healthy lifestyle is good. Try to avoid getting too heavy because obesity is associated with a higher risk of blood clots.
If you’re in the hospital, moving around is good. If your doctors have deemed that you’re at high enough risk to be on blood thinners, then make sure you don’t miss doses. Or if you’re in bed with those squeezy boots on, keep them on.
Being aware of the symptoms of blood clots and telling your doctor when you have them can also prompt doctors to investigate. Don’t be shy. Toward the end [of the guideline], we have all these questions you should bring into your provider, like “Am I at risk for blood clots? How can I decrease my blood clot risk?” We want patients to be prepared with questions they can ask their provider. If you have a proactive patient, that makes sure that everything gets taken care of.
CT: What are the symptoms of a blood clot?
STREIFF: DVTs [deep vein thromboses] are usually in the legs. They typically cause swelling. They can also cause discoloration or an aching pain in the calf or thigh. It almost feels like you have a charley horse in your calf, but it’s not transient. You can’t rub it out. And then for clots that break free from the leg and go up into the lungs, they typically cause people to have shortness of breath. Suddenly, you feel like you can’t catch your breath, or you might feel pain when you take a deep breath.
CT: When should you go to the emergency room with symptoms of a blood clot?
STREIFF: Don’t wait to hear back from your doctor if you feel really short of breath or if you or a loved one passes out. Call 911 or go to the emergency room. But let’s say you develop pain or swelling in your leg. Then I would probably call your doctor or the nurse and ask them what to do. A lot of times, we diagnose people in the clinic, and you don’t have to go to the emergency room. But anytime your symptoms feel severe or if you aren’t able to connect with your doctor, you can go to the emergency room.
CT: How are blood clots treated?
STREIFF: We use higher doses of blood-thinning medication to treat a blood clot. We use low doses to prevent blood clots. If you have developed a really big blood clot, like a big pulmonary embolism, that’s really life-threatening. Then we will also use clot-busting medications that actually dissolve blood clots. Or there are also devices to pull clots out, either with surgery or with catheters to pull the clots out of the lungs.
This interview has been edited and condensed for clarity.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.