William G. Nelson, MD, PhD Photo by Joe Rubino
ONE-STOP SHOPPING HAS ENTERED the world of cancer therapy as newly diagnosed cancer patients take advantage of multispecialty clinics and multidisciplinary treatment plans. Now, new technologies known as theranostics are poised to take the one-stop paradigm to a higher level by combining and coordinating diagnostic imaging and cancer treatment into an integrated assault on specific targets on cancer cells.
The word theranostics is derived from the Greek words therapeuein (to cure or treat medically) and gnosis (knowledge). The basic idea is that an imaging agent can be paired with a treatment so that not only can the location and extent of a cancer be ascertained, but the presence or absence of a treatment target can also be determined. In this way, the potential benefits and side effects of targeted therapies can be anticipated for individuals with certain types of cancer.
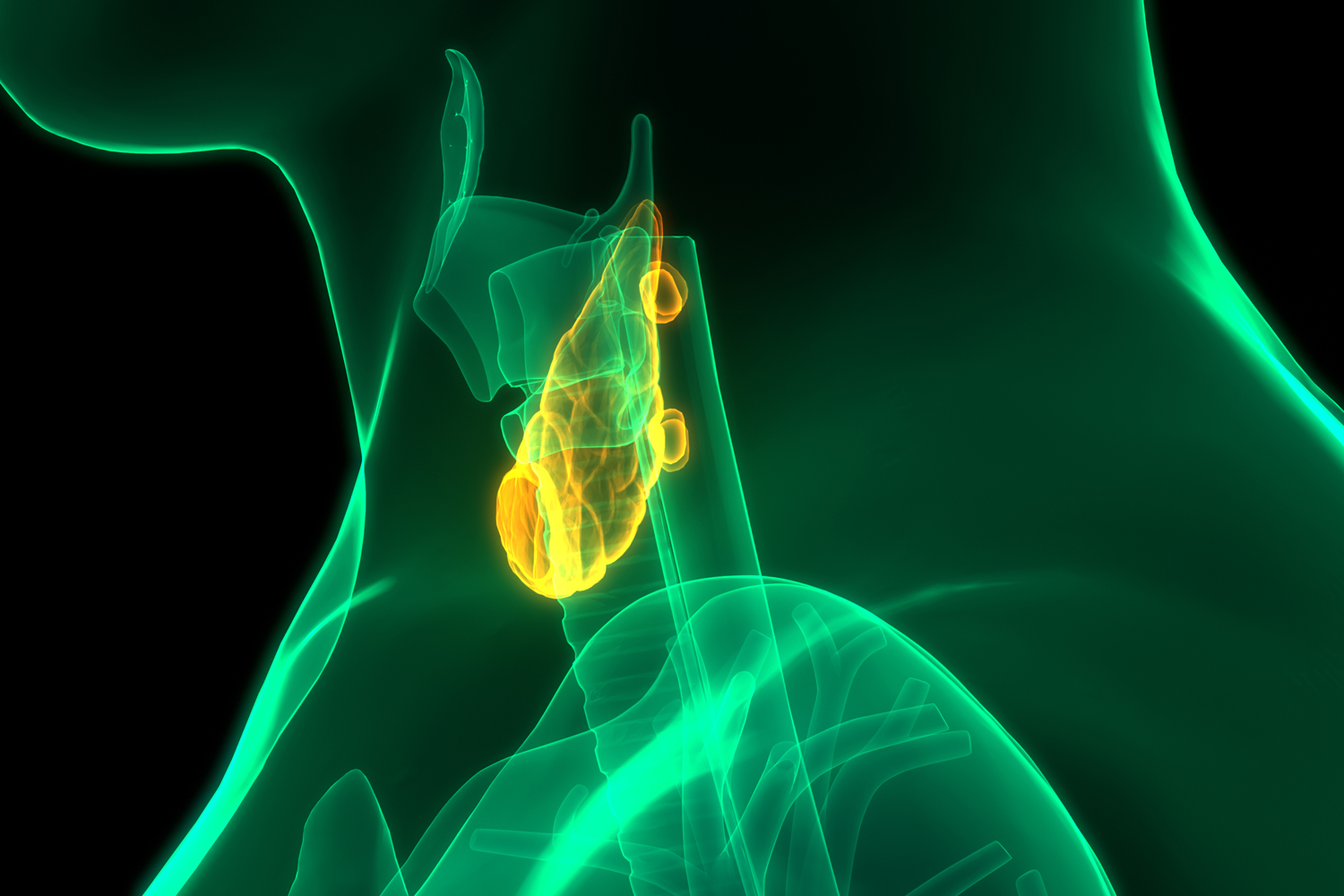
The first theranostic approach to cancer came in the 1940s with the use of radioactive iodine for finding and treating thyroid cancer. Normal and cancerous thyroid cells take up iodine in different amounts using a specialized protein on the cell surface called the sodium/iodide symporter (NIS). All but one of the 37 known isotopes of the element iodine undergo radioactive decay, with many emitting subatomic particles that can be detected for imaging or used to damage and kill thyroid cancer cells.
One radioactive iodine isotope, 131I, can be used both for scanning and treatment. For imaging, a small quantity of 131I is administered orally or intravenously to reveal whether a suspicious nodule in the thyroid takes up iodine and whether thyroid cancer has progressed to an advanced state or metastasized to distant sites. If the thyroid cancer “lights up” on the scan, a much larger dose of 131I can be given later to destroy the cancer cells. Normal thyroid cells also light up, indicating that 131I treatment damages the thyroid gland. For this reason, people treated for thyroid cancer must take a thyroid hormone supplement after iodine treatment for the rest of their lives.
The Oct. 31, 1949, issue of Life magazine featured the remarkable story of Bernard Brunstein, the first adult to be cured of thyroid cancer by radioiodine. Today, paired imaging of iodine uptake and radioactive iodine treatment for thyroid cancer remain mainstays of treatment, but theranostic pairs are also part of standard practice for imaging and treating prostate cancer, certain neuroendocrine tumors, neuroblastoma and non-Hodgkin lymphoma. Most often, theranostic pairs use different radioisotopes for imaging and treatment, unlike for thyroid cancer. With the explosion in the discovery and development of antibodies against a variety of cancers, theranostic pairs of antibodies carrying imaging radioisotopes and therapeutic radioisotopes or cytotoxic drugs are being explored as precision cancer medicine strategies.
Future theranostics may encompass even more features, exploiting the targeting properties of antibodies and other small molecules for simultaneous delivery of imaging agents for scanning, fluorescent dyes to assess whether cancer has been fully removed at surgery, cytotoxic radiation or drugs, genes for gene therapy, or nanoparticles containing various payloads. If the next generation of theranostics can detect, diagnose and treat cancer all at once with great precision and fewer side effects or complications, one-stop shopping will truly have come to cancer therapy.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.