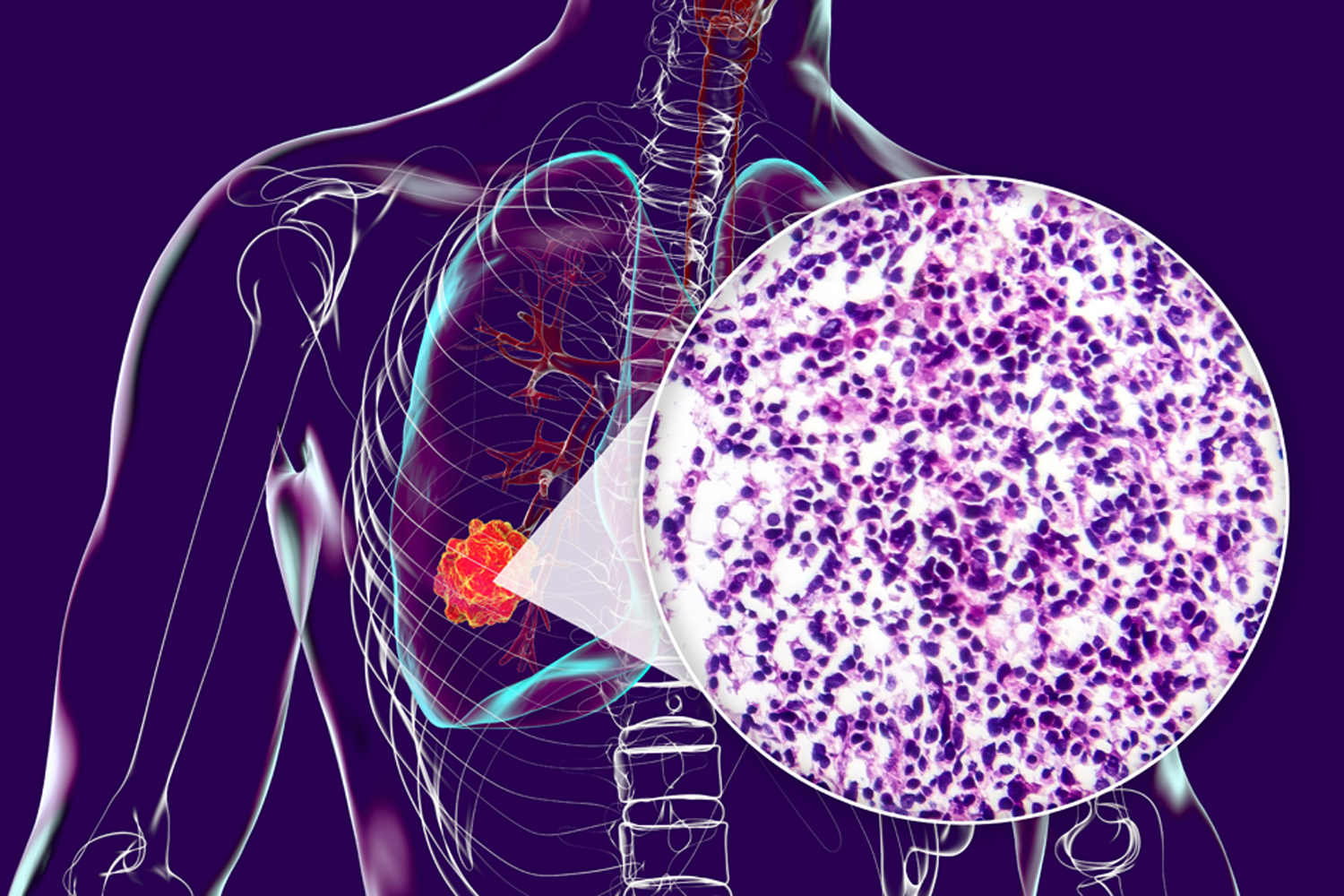
LUNG CANCER REMAINS the leading cause of cancer death in the U.S., but for locally advanced or metastatic non-small cell lung cancer (NSCLC), treatment options have expanded in the past decade. Data from a clinical trial show two of these regimens used together can improve survival for people whose cancer expresses certain mutations, but the combination could come with quality-of-life trade-offs.
In August 2024, the Food and Drug Administration (FDA) approved the combination of Rybrevant (amivantamab) and Lazcluze (lazertinib) as a first-line treatment for advanced NSCLC that tested positive for either of two specific EGFR mutations. This approval was based on data from the phase III MARIPOSA trial, published June 26, 2024, in the New England Journal of Medicine, which included 1,074 people with locally advanced or metastatic EGFR-positive NSCLC. Researchers found that people who received the combination had median progression-free survival of 23.7 months, compared with 16.6 months in those who received standard care, which was Tagrisso (osimertinib). The combination reduced the risk of disease progression or death by 30% compared with Tagrisso.
In an updated analysis presented in March at the 2025 European Lung Cancer Congress, researchers provided overall survival data from the trial. After three and a half years, 56% of the people on the combination of Rybrevant and Lazcluze were alive, compared with 44% of those in the Tagrisso group. The median overall survival of people who received Tagrisso was 36.7 months, while the median in the combination regimen group was not reached. “Patients need to know whether the progression-free survival ultimately translates into [longer] overall survival because this is what they and their physicians are most concerned about,” says trial investigator James Chih-Hsin Yang, director of the National Taiwan University Cancer Center in Taipei.
Maurice Pérol, an oncologist at the Léon Bérard Cancer Center in Lyon, France, who was not involved in the study, says that the combination made a measurable difference in cancer response. “But that clinical relevance has come at the cost of a significant increase in toxicity that requires aggressive management and may impact daily quality of life,” he says.
Scientists expected an increase in side effects from the Rybrevant-Lazcluze combination compared with using either drug alone or Tagrisso. However, researchers found that 37% of those who took the combination experienced blood clots in their veins or lungs. “We would expect about 11% of patients to have this side effect, so that was a surprise,” Yang says. Doctors can give blood thinners alongside the combination to better prevent blood clots in these patients. (For more on blood clots in cancer treatment, see “A Safer Way to Prevent Blood Clots.”)
Infusion reactions—including fever, chills and elevated blood pressure—were also common in those who received the combination. Yang says these reactions can be managed by premedicating with IV steroids. In addition, he says a newer form of Rybrevant that can be injected under the skin could lead to fewer infusion reactions.
Pérol says research looking at this regimen shows a high rate of skin-re lated side effects. “Even with aggressive management, skin toxicity remains high, with approximately 38% of the patients with [moderate to severe] skin toxicity that clearly impaired their quality of life,” he says. Some of his patients who take targeted therapies experience disfiguring sores on their face and scalp and feel unable to leave their homes, he says. Skin toxicities are more likely to occur at the start of treatment when the targeted therapy is first controlling the cancer, Pérol says.
“Patients probably will have some difficulty having a normal life [with the combined regimen],” he says. The combination includes an oral pill and infusions, in addition to treatments to mitigate side effects. “But with standard-of-care Tagrisso, it’s just one pill per day, so working and leading a normal life is easier, even if Tagrisso’s duration of response is clearly shorter than for the Rybrevant-Lazcluze combination,” Pérol says.
Yang says he has been able to manage skin toxicities in patients with antibiotics, sun avoidance, and the use of special creams and lotions. “We can’t reduce severe side effects to zero, but they can often be minimized,” he says. “In Asia, we have a lot of experience dealing with these side effects using prior generations of [drugs that are similar to Lazcluze].” Doctors can also reduce the Rybrevant dose if needed—and even stop the drug and continue with Lazcluze alone, Yang says.
Pérol notes the combined regimen, which was approved but wasn’t available to his patients in France at the time of the interview, might be an option for people with poor prognoses, including those whose cancer has spread to the brain. For these patients, he often prescribes a regimen that received FDA approval in February 2024: Tagrisso plus plati num-based chemotherapy, which carries a different side effect profile. “The overall toxicity may be greater, but it doesn’t last as long, and we have more experience managing the chemotherapy toxicity to get that patient to a better quality of life while on treatment,” Pérol says.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.