Update: On Feb. 27, 2021, the Food and Drug Administration (FDA) issued an emergency use authorization for a third COVID-19 vaccine, this one made by Johnson & Johnson. On April 13, 2021, the FDA and Centers for Disease Control and Prevention recommended a pause on the use of the Johnson & Johnson vaccine after a small number of recipients developed a rare blood clotting disorder. On April 23, the agencies recommended that use of the vaccine resume while noting that women under 50 should be aware of the risk and that there are other COVID-19 vaccines available.
Most health care providerS are familiar with triage, the careful and intentional orchestration of patient care to ensure that those who have the most severe injuries or illnesses get care quickly and appropriately. This routine health care practice has taken on added complexity as many hospitals and other care facilities continue to struggle with a COVID-19 surge, all at the same time as COVID-19 vaccines are beginning to become available.
At the Cleveland Clinic Taussig Cancer Institute, an average of four out of every 20 patients who were hospitalized for leukemia at the end of November 2020 were testing positive for COVID-19, estimates hematologist-oncologist Mikkael A. Sekeres, up from one to two out of 20 during the first surge in spring 2020.
For More Information
Read more coverage here from Cancer Today on the various impacts of the coronavirus on people with cancer.
“Our toggle point in triaging patients was whether or not they were dependent on oxygen,” says Sekeres, describing the challenge of treating cancer patients who were infected with the coronavirus. All patients admitted to the hospital were being tested for the virus. Patients who tested positive for COVID-19 but didn’t require oxygen or have major symptoms related to coronavirus infection would be treated on the leukemia floor. “Our rationale was that if they are being admitted to the hospital, their leukemia symptoms were predominating—but they just happened to test positive for COVID,” Sekeres says. If a patient tested positive for COVID-19 but needed oxygen, they would be admitted to the COVID-19 floor.
Sekeres, who recently started a new position as the chief of the division of hematology at the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine, notes that a dual diagnosis of COVID-19 and leukemia adds an almost dizzying complexity to patient care. “Acute leukemia is one of the few cancers that hits somebody fast and furiously,” says Sekeres. “And the only way you are going to get on top of it is to treat it.” Thus, it’s possible and even good clinical practice for a leukemia patient who has COVID-19 to be admitted to the intensive care unit for symptoms related to COVID-19 and still receive chemotherapy, Sekeres says.
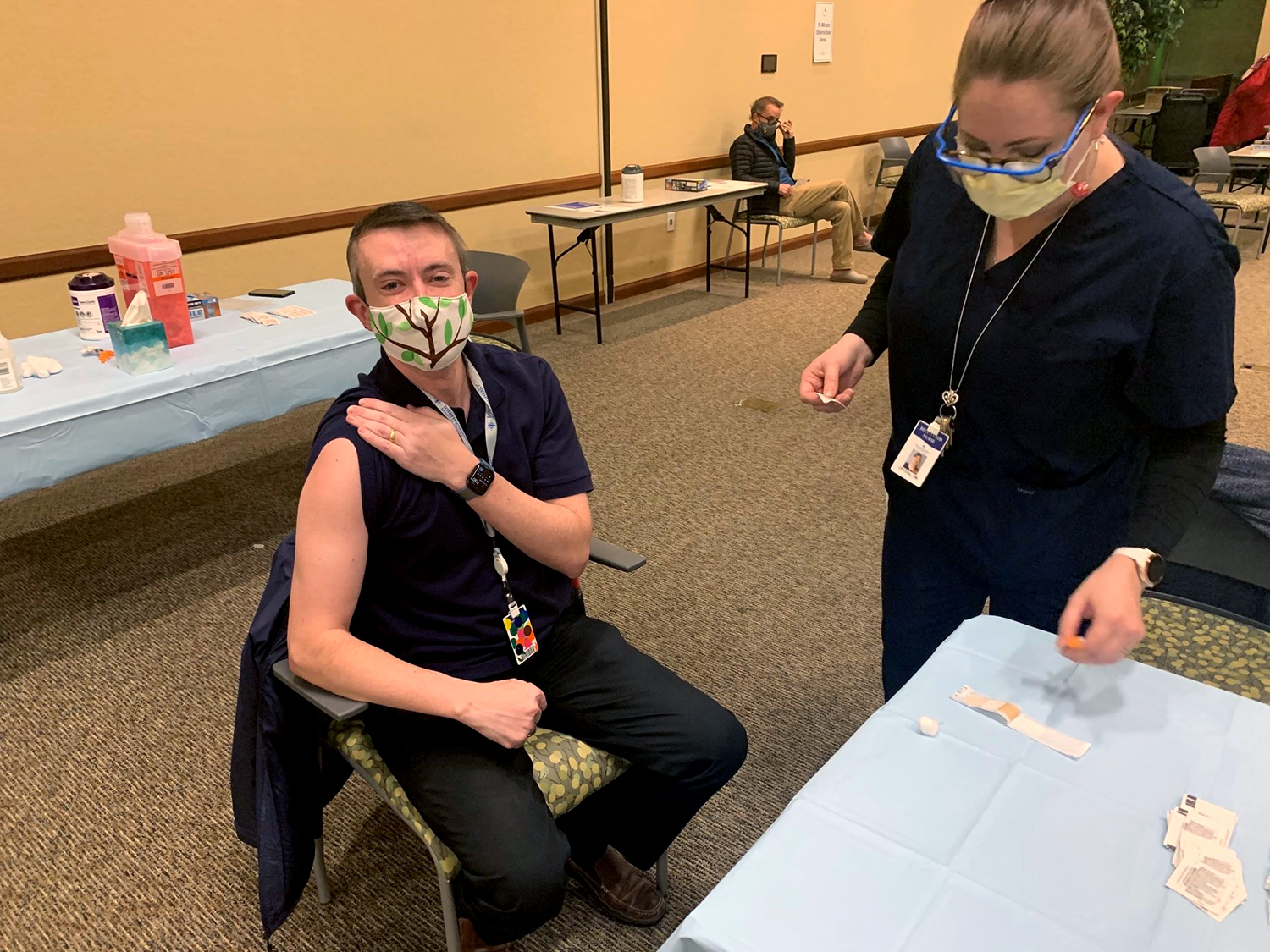
The logistics of caring for patients with cancer in a pandemic hasn’t gotten easier, even as many health care workers feel a gleam of hope as they roll up their sleeves to receive one of the two COVID-19 vaccines—the Pfizer-BioNTech vaccine or the Moderna vaccine—that are currently available as part of a phased national distribution plan. In fact, the arrival of these vaccines, which were authorized for emergency use by the Food and Drug Administration in December, poses a new triage challenge as states and local authorities grapple with who should receive vaccination first with limited supply.
Should Cancer Patients Be Prioritized?
On Dec. 20, 2020, a committee of the Centers for Disease Control and Prevention (CDC)—the Advisory Committee on Immunization Practices (ACIP)—updated criteria for prioritizing certain groups in vaccine distribution. ACIP’s initial prioritization started with a phased rollout to health care workers and residents in long-term care facilities and then to people who are 75 and older and certain essential workers. Following vaccination of these first two groups, ACIP suggested expanding distribution to those 65 and older as well as those 16 and older who have medical conditions, such as cancer, that increase the risk of severe COVID-19. However, on Jan. 12, former Health and Human Services Secretary Alex Azar in a press briefing advised states to make vaccines available for anyone who is 65 and older, as well as those with comorbidities. States and other local jurisdictions ultimately have the say in how they distribute their vaccines—including when they prioritize people with high-risk medical conditions.
Stressing research that supports an elevated risk of mortality for patients with cancer who are infected with COVID-19, the American Association for Cancer Research (AACR) issued a position paper Dec. 19, 2020, in the journal Cancer Discovery urging vaccination priority be given to all patients in cancer treatment or those with advanced cancer. (The AACR publishes Cancer Today.) The paper pointed out that patients with hematologic malignancies and lung cancer should especially be considered for prompt vaccination, given multiple studies that suggest an increased risk for these patients of suffering serious outcomes from COVID-19. In addition, on Jan. 22, the National Comprehensive Cancer Network (NCCN), an alliance of cancer centers that publishes guidelines for cancer care, provided further recommendations, affirming that cancer patients should be prioritized for vaccination and noting that vaccination is recommended for all cancer patients, household contacts and caregivers.
A study published Dec. 10, 2020, in JAMA Oncology analyzed patient electronic health records from 73.4 million patients across the United States through Aug. 14, 2020. Those who had a recent cancer diagnosis were at significantly increased risk for COVID-19 infection, and the association was strongest in patients with leukemia, non-Hodgkin lymphoma and lung cancer. In addition, a meta-analysis published Nov. 2, 2020, in the Journal of the National Cancer Institute combined data from three studies to calculate that the case fatality rate among hospitalized patients who had cancer and COVID-19 was 23.4%, compared to 5.9% for patients without cancer who were also hospitalized with COVID-19 symptoms. Using data from additional studies, the researchers found that the case fatality rates were even higher in lung and hematologic cancer patients with COVID-19, at 32.9% and 34.2%, respectively.
“This is just my interpretation of the data, but it appears to me that the lead driver of excess deaths among cancer patients who get COVID-19 are those who have hematologic malignancies,” says Sekeres. “I would certainly make the case that people who have compromised immune systems with cancer should be prioritized in receiving the vaccine.”
Still, it’s not known if the COVID-19 vaccines will elicit a strong enough immune response in cancer patients to reach the levels of vaccine efficacy seen in clinical trials, particularly in patients whose cancers affect the white blood cells that form a primary defense as part of the immune system. In addition, chemotherapy and other treatments for cancer can cause neutropenia. This condition, in which white blood cells become depleted, can make people more susceptible to getting infections and potentially reduce the immune response to vaccines.
The Food and Drug Administration has so far authorized two vaccines for COVID-19.
Currently two COVID-19 vaccines have been given emergency use authorization by the Food and Drug Administration. These vaccines, developed by Pfizer-BioNTech and Moderna, have been shown to be 95% and 94% effective, respectively, at preventing people from becoming sick with COVID-19 in clinical trials.
The Pfizer-BioNTech vaccine, first granted authorization for use on Dec. 11, is administered in two shots 21 days apart for people age 16 and over. The Moderna vaccine, approved on Dec. 18, is given in two shots 28 days apart for people over age 18.
So far, the safety protocols for mitigating the potential transmission of the virus are largely the same for the vaccinated as the unvaccinated, since research shows the COVID-19 vaccines reduce the likelihood of getting sick from COVID-19, but the degree to which they reduce a person’s ability to transmit the virus is not yet known. This may change as more data emerge.
Both of these vaccines use messenger RNA, which give instructions to cells to make the spike protein that is on the surface of the coronavirus. The vaccine prompts a person’s cells to make just part of the virus so that it elicits an immune response, says Monika Shah, an infectious disease specialist at Memorial Sloan Kettering Cancer Center in New York City. “It’s like an instruction manual for the cell to make a protein and get an antibody response,” she says.
If a vaccinated person’s immune system encounters the virus in the future, it should already recognize it and be able to more readily fight it off.
The Search for Guidance
The clinical trials testing the two available COVID-19 vaccines did not include cancer patients who had suppressed immune systems, says Monika Shah, an infectious disease specialist at Memorial Sloan Kettering Cancer Center in New York City. “Most of these vaccine trials do exclude people who are immunocompromised because they want to see if it works in healthy people first,” she says. In fact, just 3.7% of people had cancer in the Pfizer-BioNTech trial that led to the vaccine’s emergency use authorization. The trial excluded people taking immunosuppressive treatments for cancer, per usual trial protocols.
The two COVID-19 vaccines approved so far use messenger RNA (mRNA), a type of molecule that provides instructions to cells on what proteins they need to make at any given time. Once the mRNA from one of these vaccines enters a person’s cells, it causes them to temporarily produce a protein known as the spike protein, which is also found on the surface of the coronavirus. After vaccination, the immune system starts making antibodies that help fight the coronavirus if infection occurs. The mRNA doesn’t interact with DNA or have the potential to infect a person with COVID-19, Shah says. “From a safety perspective, we have no reason to think at all right now, based on how these two vaccines are made and what they are comprised of, that there really is any safety concern. You cannot get COVID from this vaccine. That is true for both non-cancer patients and vaccine recipients, as well as cancer patients considering getting the vaccine.”
When deciding whether a cancer patient should receive the vaccine, Shah notes, there isn’t a one-size-fits-all approach. Patients taking hormone therapy or targeted therapy may have different experiences than those taking chemotherapy, she says. “A person who has a solid tumor is going to be different than somebody who has leukemia or lymphoma,” she says. “There is a chance, of course, in patients with leukemia or lymphoma, that they may not have as robust an immune response to the vaccine. Of course, that’s theoretical, but it’s something we could expect. A lot of it depends on personal circumstances and personal therapies, and a discussion with your health care provider about the risks and benefits.”
Shah does not recommend delaying urgent treatment just to get the COVID-19 vaccine, but she does mention there may be optimal windows for patients to get the COVID-19 vaccine while undergoing treatment. The NCCN guidelines suggest that patients with hematologic malignancies who are receiving chemotherapy delay receiving the vaccine until their absolute neutrophil count, which is a measure of white blood cells and immune function, returns to a normal level, for instance. However, the NCCN states that patients receiving chemotherapy, targeted therapy, immunotherapy or radiation for solid tumors should get the vaccine as soon as it is available to them.
Shah also relies on safety and efficacy data from studies of previous vaccines to guide her recommendations. “In general, we recommend flu shots annually for most of our patients with cancer,” she says. “Now, we know some of them won’t respond, but we still recommend it. And we do that because when you get the flu vaccine, even if you don’t have a full response, you may actually have less severe disease. So that would be a reason to get the [COVID-19] vaccine even if, in theory, you might not have as robust of an immune response.”
Recent findings suggest that certain cancer patients, such as blood cancer patients, may have a poor immune response to the virus. For example, one research letter published in the Dec. 24, 2020, New England Journal of Medicine indicated that patients with blood cancer who received stem cell transplants or CAR-T cell therapy may have a decreased immune response to the coronavirus. The study noted these patients could shed the virus for longer than two weeks. Another study, published Jan. 5, 2021, in Cancer Cell, suggested that patients with blood cancer who get COVID-19 may have different immune signatures than other infected cancer patients, who have an immune response similar to that of people without cancer. This could be a sign that blood cancer patients do not launch as effective and lasting an immune response to the coronavirus as others, which theoretically might mean that they may not launch as strong an immune response to the vaccine as others.
However, in Sekeres’ mind, these research findings support giving the vaccine to patients with hematologic malignancies, specifically. “I would certainly make the case that people who have compromised immune systems with cancer should be prioritized in receiving the vaccine,” he says. “In a patient population where the death rate from infection is four times higher than for other populations, in my mind, ethically, it’s worth the risk that the vaccine may not work if we have a decent chance of preventing those deaths.”
As a health care provider, Sekeres received his first of the two doses of the vaccine on the first day at his new institution, Sylvester Comprehensive Cancer Center in Miami. Since then, his cancer center has also started offering the COVID-19 vaccine to patients 65 and older who are undergoing cancer treatment. Memorial Sloan Kettering in New York City, where Shah works, also started offering vaccination to New York cancer patients 65 and older in active treatment. The Cleveland Clinic has started vaccinating patients age 80 and older in its Ohio location and 65 and older in its Florida locations.
Setting an Example
As a health care provider, Mark Lewis, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, was among the first in his state to receive a COVID-19 vaccine on Dec. 18. Lewis, a cancer survivor who was diagnosed with pancreatic neuroendocrine tumors when he was 30 years old in 2009, admits he felt guilty receiving the vaccine before some of his patients. In December 2020 and January 2021, he tweeted pictures of himself receiving the vaccine, along with a series of lighthearted memes. He hopes sharing his pictures and perspectives on social media will help build his patients’ confidence in getting the vaccine when the time comes for them.
Like many health care providers, Mark Lewis, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, took the opportunity to share the news of his first vaccination on social media. On. Dec. 18, 2020, he tweeted, “Dear Santa, You can skip me this year. I’m good.” Photo courtesy of Mark Lewis
Lewis can’t think of many reasons why his patients in his outpatient clinic shouldn’t get the vaccine, beyond contraindications that apply to everyone, like an allergy to a vaccine ingredient. Some cancer patients are nevertheless deciding to wait. Shonte Drakeford, who was diagnosed with metastatic breast cancer in 2015 when she was 31, says she wants to see more data prior to getting vaccinated—particularly in people who have metastatic disease and are African American like her. The study from Pfizer-BioNTech enrolled more than 43,000 people, including 26% Hispanic/Latino, 10% Black, 5% Asian and 1% Native American participants. Of the more than 30,000 people who participated in the Moderna vaccine trial, approximately 20% were Hispanic/Latino, 10% were Black, 5% were Asian and 1% were Native American. The racial and ethnic makeup of the U.S. population, using data from the U.S. Census Bureau, breaks down similarly: 19% Hispanic/Latino, 13% Black, 6% Asian and 1% American Indian or Alaska Native.
Drakeford is a nurse practitioner who does virtual consults one day a week for a small primary care practice in Upper Marlboro, Maryland. She says that as a stage IV cancer patient, she adhered to social distancing practices as a matter of course long before these practices became a worldwide imperative. The 36-year-old’s treatment regimen, which includes Ibrance (palbociclib) and letrozole, has kept her cancer in check for more than five years, but it also depletes her white blood cell counts.
“I’d rather just wait six months to a year until the vast majority of the population has gotten it and I have a little more data and information because, at this point, it won’t really change the way I live,” she says.
Sheri Baker, who has been in treatment for multiple myeloma, a type of blood cancer, for almost a decade, sees it a little differently: “Why wouldn’t I get it?” asks the 58-year-old from Meridian, Idaho. Baker is hoping a vaccine will become available sooner now that her state has lowered age restrictions to 65. “I am tired of having to be careful, not go anywhere, not have family gatherings. I want to travel again,” Baker says, adding that the more people who get vaccinated, the closer all people will get to a sense of normalcy. “And although we do not know the level of protection it will give us as patients on treatment, some protection is better than no protection.” It’s not yet known whether the vaccine prevents transmission of the coronavirus, so the CDC still stresses that people who are vaccinated continue to practice social distancing and wear masks.
However, for the first time in a long time, health care providers and patients seem hopeful. “The way I think about this right now is that I feel there’s a little glimmer of light right now towards the end of a very dark and windy tunnel. No, we’re not at the end of that tunnel right now, but I can see a little bit of light,” says Shah.
The hope of health care providers who were first in line to receive the COVID-19 vaccine is that their willingness to receive the vaccine will prompt patients to do the same as supplies increase.
“I have told my patients that I’m getting vaccinated because I want them to know that I think I’m going to be here to take care of them,” Lewis says. Some of his patients were overjoyed when he shared the news of his vaccine. “It was actually really touching. One patient wanted me to go first because he wanted me to be around, not just around as in being alive, but also to just be here in the hospital, not in quarantine, so I can take care of him. So, in some ways, that mitigates any guilt I have—that I might be of service to my patients.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.





