ON THE TOPIC OF IMMUNOTHERAPY, there is no shortage of compelling stories about incredible cancer remissions. One article describes a melanoma patient’s grapefruit-sized tumor melting away within weeks of treatment. In another example, a 76-year-old man finds an answer to an otherwise untreatable advanced bladder cancer by daring to ask whether an experimental treatment that unleashes the immune system against cancer might help him.
The dramatic successes of immunotherapy open a new path for treating cancer. Compared with other treatments, such as surgery, radiation and chemotherapy, that are directed at cancer itself, immunotherapy spurs the body’s own defenses to action. The U.S. Food and Drug Administration (FDA) approved the first checkpoint inhibitor, Yervoy (ipilimumab), in 2011 for the treatment of metastatic melanoma, and other immunotherapy drugs followed. As of November 2019, the FDA had approved seven checkpoint inhibitors to treat 16 different cancer types; one of these checkpoint inhibitors can also be used to treat any cancer type so long as it carries a certain tumor biomarker. Checkpoint inhibitors target certain proteins on T cells to help them lift the brakes on the immune response to cancer cells.
Despite the excitement over this new way of treating cancer, however, the unfortunate reality is that checkpoint inhibitors and other types of immunotherapy work in only a fraction of people with cancer. One study published May 3, 2019, in JAMA Network Open estimates that about 44% of patients in the U.S. with cancer are now eligible for treatment with checkpoint inhibitors, but only about 13% of those eligible patients respond to the drugs. In general, checkpoint inhibitors are more likely to work for patients with cancers that have acquired many mutations. The presence of these abnormalities makes it easier for the immune system to spot and attack the cancer. Cancer types that have responded to checkpoint inhibitors include advanced melanoma, non-small cell lung cancer, and cancers of the kidney and bladder. In other malignancies, including pancreatic, ovarian, and brain cancer, the benefits of immunotherapy, for the most part, remain to be seen.
“The main issue we have now is to try to figure out why the majority of patients do not have a benefit in terms of survival when treated with immunotherapy,” says Joseph Ciccolini, a clinical pharmacologist at the University Hospital of Marseille in France, who studies nanoparticle delivery of a variety of anti-cancer agents so they can better reach tumors. Ciccolini and other researchers note that many tumors are “cold,” meaning that the immune response to the cancer isn’t strong enough for checkpoint inhibitors to make a difference.
“We need to find ways to make more tumors respond to treatment,” Ciccolini says, “to turn a ‘cold’ tumor into a ‘hot’ tumor.”
The Roots of Resistance
To understand why immunotherapies don’t work well for all cancers, it is helpful to consider why our immune system fails to fight cancer in the first place. The immune system has a variety of mechanisms and cell types to identify and attack foreign invaders, primarily bacteria and viruses. T cells that recognize, find and destroy these invaders make up one part of the body’s defense. The trouble is that cancer cells originate from the body’s own cells. To protect against cancer, the immune system must recognize cancer cells as harmful. Even when it does so, tumors are often remarkably good at dampening immune responses, thus protecting themselves at the expense of the rest of the body.
Getting to the bottom of why certain cancers don’t respond to immunotherapy and how to increase their response is the primary mission of the Beatty Lab at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. A medical oncologist and researcher, Gregory L. Beatty studies pancreatic cancer, which has a five-year survival rate of less than 10%. More than 56,000 people in the U.S. were expected to receive a diagnosis of pancreatic cancer in 2019, while close to 46,000 people were expected to die from the disease in that year.
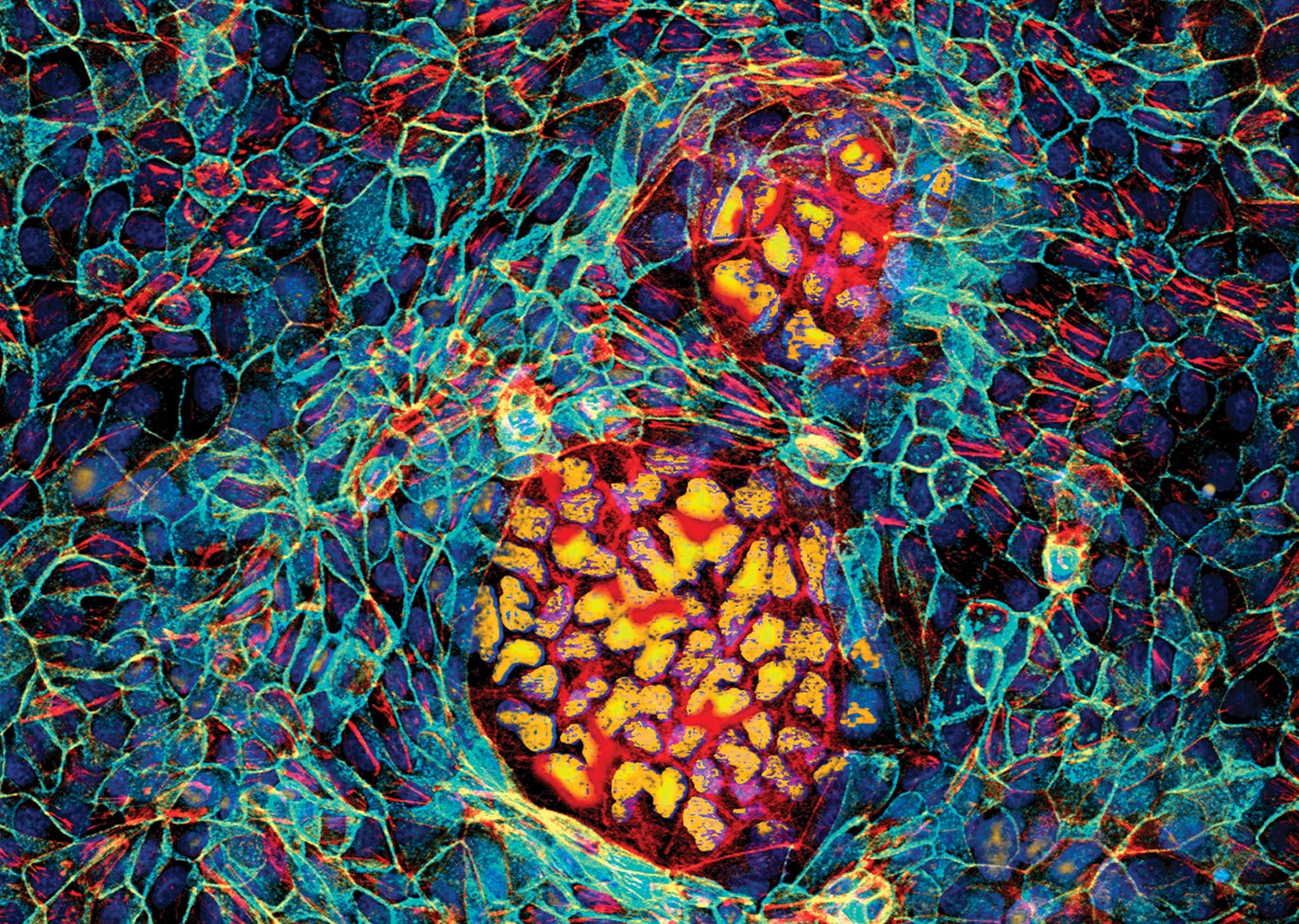
The stubborn resistance of pancreatic cancer to all forms of treatment, including immunotherapy, is precisely what piqued Beatty’s research interest. Pancreatic cancers often are loaded with immune cells called macrophages. Rather than help to fight the cancer, however, those macrophages get co-opted to help the cancer grow, spread and resist treatment in ways that are still not fully understood.
Most pancreatic cancers contain few if any T cells, the kind that are good at destroying cancer cells. Studies show that people whose pancreatic cancers do include some T cells tend to fare better than others, Beatty says, offering a glimmer of hope that immunotherapy might one day treat pancreatic cancer too. However, these T cells often get trapped in the surrounding tissue, where they interact with macrophages and connective tissue but not with the cancer, he says.
“It’s not clear what they are actually doing,” Beatty says. “They’re not activating, not dividing, not making proteins needed to kill a tumor cell.” In fact, he says, in studies of mice, engineered T cells designed to target pancreatic cancer have been found to rapidly become dysfunctional.
In addition, blood samples taken from people with pancreatic cancer show weakened immune function, with T cells that didn’t divide in the same way as healthy immune cells do. Asking those T cells to fight cancer, Beatty says, is like asking a person to run a 100-meter dash with both legs tied together. “You’re asking less fit T cells to do a difficult job, to find and kill the tumor,” Beatty says.
Pancreatic cancers, then, appear to derail the immune system in several ways. To overcome this, researchers need to figure out ways to combine strategies and therapies, Beatty says.
Combining Therapies
Breast surgical oncologist and immunologist Elizabeth Mittendorf is exploring similar issues in her lab at Dana-Farber Cancer Institute in Boston by looking at how standard and experimental therapies influence the immune environment within breast tumors. “When you look at a breast tumor under the microscope, you don’t [generally] see a significant number of lymphocytes or T cells that recognize something as foreign, attack and destroy,” she says. “It suggests [breast tumors] aren’t as foreign or abnormal appearing as other tumors we see.”
Breast tumors usually carry fewer mutations than some other cancer types, such as melanoma or lung cancer, making them tougher for the immune system to spot. Not surprisingly, the first clinical trials of checkpoint inhibitors to treat people with breast cancer delivered disappointing results. When used as single agents to treat metastatic breast cancer, checkpoint inhibitors showed “no significant response,” Mittendorf says, but subsequent studies have shown that immune agents used in combination with other drugs may be able to enhance the effectiveness of treatment.
“The thought was, ‘We have to do something that will increase the immune response, to augment the path forward,’” she says, describing how combining immunotherapies with standard treatments like chemotherapy and radiation might bolster immune response in breast cancers—as well as in other types of cancers. The idea is that traditional cancer treatments could damage DNA within cancer cells, causing abnormal proteins to find their way to the surface of a tumor, which could spark an immune response that checkpoint inhibitors could then help to amplify.
This treatment approach has already gained some traction with the first FDA approval of immunotherapy for breast cancer. In March 2019, the FDA granted accelerated approval to Tecentriq (atezolizumab) combined with the chemotherapy drug Abraxane (nab-paclitaxel) as a first-line treatment for some women with advanced triple-negative breast cancer, based on results from a trial with more than 900 women. The treatment is indicated for women who cannot be treated surgically and who have locally advanced or metastatic triple-negative breast cancer that tests positive for a protein called PD-L1, which helps cancer cells hide from the immune system.
Many researchers are exploring the potential of other combination approaches with immunotherapy for breast cancer. In a review in the August 2019 JAMA Oncology, Mittendorf reported that more than 290 clinical trials were underway to test the use of immunotherapies to treat breast cancer. Many of those trials are evaluating the use of checkpoint inhibitors delivered in combination with chemotherapy, targeted treatments, vaccines or other treatments.
“I think we’re turning a corner in breast cancer,” Mittendorf says. “We may see additional [immunotherapy] agents approved in combination with chemotherapy and in different settings—not just in metastatic cancer but also earlier in the disease.”
Mittendorf recently published clinical trial results of another immunotherapy approach: a vaccine called NeuVax (nelipepimut-S) given after breast cancer treatment to prevent a cancer recurrence. The vaccine is designed to build immunity to a protein called HER2, which is found on the surface of many aggressive breast cancers. Earlier studies showed the vaccine was well tolerated and appeared to build immunity to HER2 in patients with HER2-positive breast cancers. But the phase III trial, which included 758 patients with early-stage breast cancer, ended in failure; those who received the vaccine weren’t significantly protected from recurrence. Mittendorf says that’s not the end of the story. There’s also interest in combining the vaccine with other treatments, including checkpoint inhibitors.
“Checkpoint blockade is designed to take the brakes off of T cells,” she says. “The vaccine can stimulate T cells” to recognize cancer and then checkpoint inhibitors could help to unleash the T cells.
Insights From Clinical Trials
At the University of Texas MD Anderson Cancer Center in Houston, a team that includes medical oncologist and immunologist Padmanee Sharma and immunologist James P. Allison continues to devise strategies aimed at broadening immunotherapy’s effectiveness to more cancers and more people with cancer. (Allison was awarded the Nobel Prize for Physiology or Medicine in 2018 for his work in discovering an antibody that would become the first approved checkpoint inhibitor.)
Now Allison and Sharma have developed a platform to capitalize on the many ongoing clinical trials on checkpoint inhibitors, including those focused on their use in tumors of the bladder, prostate and kidney.
“In the immune checkpoint field, there are so many trials,” Sharma says. The question is “how can we take advantage of trials to understand the human response that’s hard to model in mice?”
To answer their own question, Sharma, Allison and colleagues are collecting tumor and blood samples at multiple time points from patients receiving experimental immunotherapy treatments in more than 100 clinical trials at MD Anderson and looking for changes that occur following treatment. They hope to isolate factors that make a difference in a cancer that responds to immunotherapy and a cancer that doesn’t.
Thus far, their research has shown that treatment with the checkpoint inhibitor Yervoy increased the activity of an enzyme called EZH2 in T cells. They found that some patients with prostate cancer also have higher levels of EZH2 in tumor cells and have poorer responses to immunotherapy. This poor response prompted Sharma to design a clinical trial testing Yervoy and an experimental treatment that inhibits EZH2 for people with prostate cancer—as well as patients with bladder and kidney cancer—whose disease did not respond to other checkpoint inhibitor treatment.
Allison and Sharma have also found evidence that checkpoint inhibitor treatment in prostate cancer spurs a secondary brake, a more recently discovered checkpoint regulator called VISTA. This mechanism may explain why checkpoint inhibitors generally haven’t worked in prostate cancers and could lead to the development of new agents for treating prostate cancer alongside existing treatments.
“The clinical piece takes time,” Sharma says. “We have to convince companies to work together. There are issues of safety in combining new agents. There are things to work through. But the science speaks for itself. We are able to use this platform to identify relevant pathways and design the next set of trials that will be meaningful.”
A variety of immunotherapy approaches are now used to treat cancer.
Treatments designed to boost the immune system’s ability to fight cancer work in a variety of ways. Here are some of the approaches:
Checkpoint inhibitors amplify existing immune responses by releasing the molecular brakes that keep those responses, and especially T cells, in check.
Treatment vaccines introduce specific antigens—short bits of protein, for example—to elicit the production of an immune response against proteins found on cancerous cells already in the body. Some vaccines are customized from a person’s tumor cells, while others are engineered using specific substances that can be found on the surface of tumor cells. One such cancer treatment vaccine, Provenge (sipuleucel-T), uses immune cells taken from the blood to treat metastatic prostate cancer.
Viral therapy uses a genetically modified virus to infect cancer cells, which causes them to burst and release cellular contents to alert the immune system. Imlygic (talimogene laherparepvec), which is also called T-VEC, contains a genetically modified cold sore virus that can be injected into inoperable melanoma lesions in the lymph nodes or skin.
CAR-T cell therapy involves collecting the patient’s blood and genetically modifying his or her T cells in the lab to produce a receptor that recognizes and binds to an antigen found on the surface of cancer cells. Those modified cells are reproduced in large numbers before being infused back into the patient, either intravenously or at the tumor site. Two CAR-T cell therapies, Yescarta (axicabtagene ciloleucel) and Kymriah (tisagenlecleucel), are approved for certain blood-related cancers.
Reasons for Hope
Clinical progress continues to be made slowly but surely. As a result of these continued efforts, more patients are seeing benefits. After her diagnosis with triple-negative inflammatory breast cancer in 2013, Rita McGuire O’Brien, who lives in Fall River, Massachusetts, was one of the women who enrolled in the trial that led to the landmark approval of Tecentriq and Abraxane for triple-negative breast cancer. O’Brien had surgery and treatment with chemotherapy and radiation, but none of these approaches kept her cancer in check. After her participation in the trial of the immunotherapy-chemotherapy combination in April 2015, her CT scans showed almost no evidence of cancer, with one involved lymph node that got smaller but didn’t completely go away. In September 2019, she and her doctors decided to stop chemotherapy and continue treating her with immunotherapy alone. But scans in November showed changes in the lymph node, and biopsy results indicated she had a second type of breast cancer. So O’Brien, who is 61, will add chemotherapy back to her treatment regimen.
Still, her story serves as one of those remarkable examples that offer hope for what immunotherapy might one day become for more people as the research continues to advance. After her initial diagnosis, O’Brien didn’t know what her future would hold. “My doctor told me, ‘I won’t tell you you’ve got days, but I don’t think you have years.’ And now, here I am, five years later.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.