BEYOND THE INITIAL SHOCK of a life-threatening cancer diagnosis, people typically fear chemotherapy—a treatment that conjures up visions of nausea, hair loss and an overriding sense of feeling unwell. While cancer threatens one’s life, chemotherapy threatens to erode a person’s enjoyment of life, as chemicals meant to destroy rapidly dividing cancer cells also strike fast-growing healthy cells.
When Gitte Joergensen, who was diagnosed with stage III lobular breast cancer at age 42 in 2020, went through chemotherapy treatment, she relied heavily on a coping mechanism that has always served her well: humor.
“My advice is always try and make fun. Humor is a big thing, especially when you are in these literal horror-like situations. It’s quite extreme, and you have to just crumble or be able to have a laugh at it,” says Joergensen, who was born in Denmark and now lives in Coventry, Connecticut.
Joergensen’s treatment included a double mastectomy followed by four months of chemotherapy, referred to by the acronym AC-T for the drugs’ brand names: Adriamycin (doxorubicin), Cytoxan (cyclophosphamide) and Taxol (paclitaxel). Typically, in this regimen, Adriamycin and Cytoxan are given together first, but Joergensen’s doctors adjusted the usual order of her treatment because it was the opening days of the pandemic in the U.S. She started with Taxol, which carries less toxicity than Adriamycin and Cytoxan, to try to delay any hospitalization that might occur during her treatment since hospitals were filled with COVID-19 patients.
Joergensen remembers other challenges with chemotherapy. She couldn’t buy hair clippers when she started treatment because stores were closed due to the pandemic. She notes her resourcefulness in using her cat’s electric clippers to shave her head. With a bare head and a body bloated by steroids, she poked fun at her appearance and called herself Lord Varys, a bald and rotund fictional character from the TV series Game of Thrones.
“Obviously, I was frightened,” she says, but she focused most of her energy on counting down the days until her four months of chemotherapy treatment were over. “You have to keep crossing off days in your calendar. You’ve got to be able to laugh at yourself and the situation.”
While new cancer treatments, including immune checkpoint inhibitors and targeted therapies, are touted as exciting advances with fewer side effects, chemotherapy remains a cornerstone of treatment. Typically given over weeks or months and broken into cycles of one or more treatment days followed by periods of rest, chemotherapy works by killing cancer cells. But it can also damage healthy cells, such as those in the gastrointestinal tract, the mouth, the hair and the blood. The good news is oncologists today are better able to predict the likelihood of certain side effects from chemotherapy drugs, and they have more tools at their disposal to prevent and manage these effects.
The Difference Between Night and Day
While training to be an oncologist more than 20 years ago, Nicole Kuderer, who studies treatment-related toxicities, learned from more experienced colleagues about a different reality for patients treated with chemotherapy in the past.
“From a historical perspective, things have really gotten so much better. It really is like night and day compared to the early chemotherapy days, even compared to the ’80s and ’90s,” says Kuderer, who is the medical director of the Advanced Cancer Research Group, an independent research collaborative based in Kirkland, Washington, that focuses on cancer toxicities. Oncologists who have practiced medicine for many decades still remember when people kept buckets by their bedside and were routinely admitted to the hospital, she says. Although chemotherapy is still a difficult treatment, most people make it through without a hospital admission, and fewer patients experience nausea or vomiting.
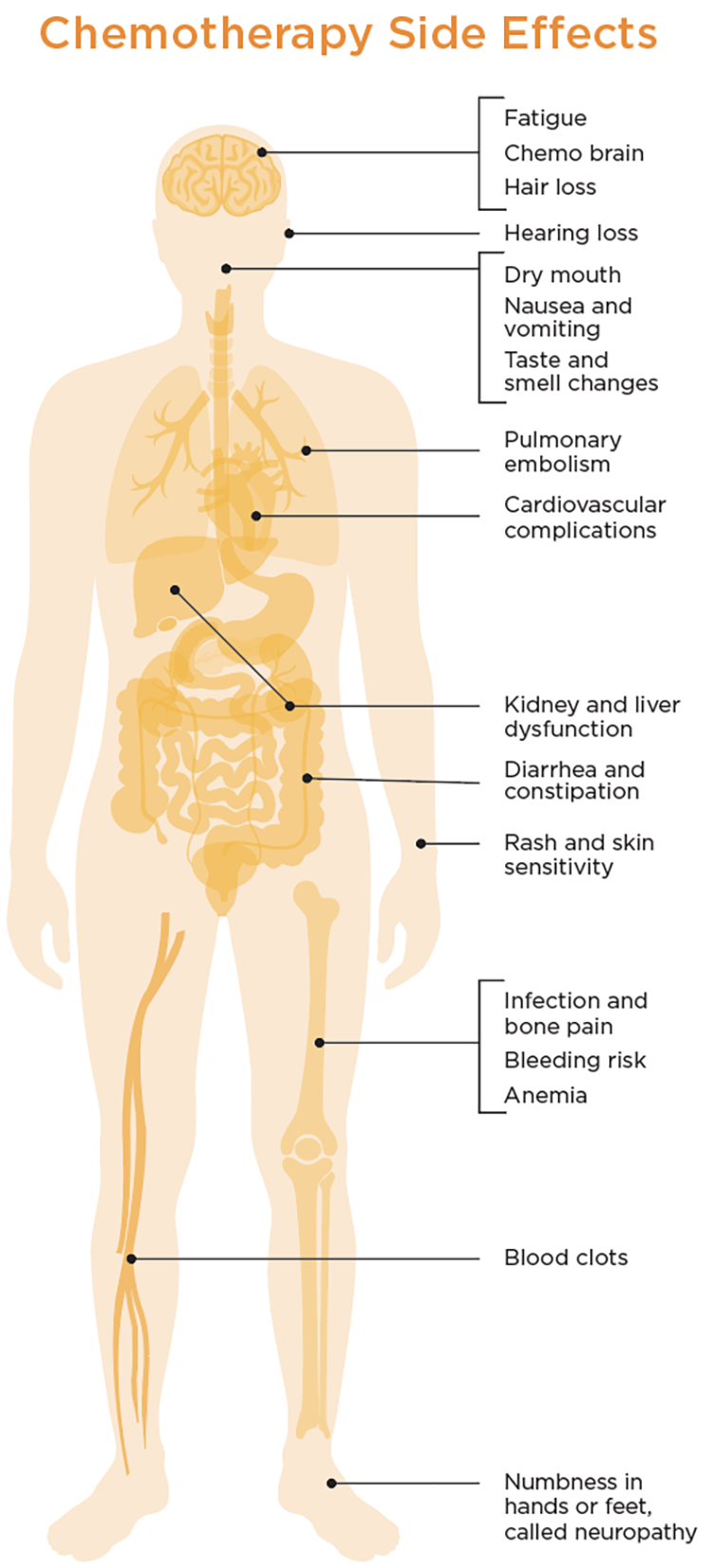
This illustration highlights potential side effects of chemotherapy, but each patient’s experience will vary. Adapted from Nature Reviews Image by Pikovit / WinWin artlab / Shutterstock.com
There are dozens of chemotherapy drugs used to treat various types of cancer, and while the basic classes of chemotherapies have remained largely the same over the years, drugs to manage many of the side effects have gotten better. When treating patients, oncologists rely on their experience and guidelines from professional organizations like the American Society of Clinical Oncology, the American Society of Hematology and the National Comprehensive Cancer Network to guide them in using these drugs to help reduce chemotherapy’s ill effects. The risk of developing side effects differs depending on the type of cancer and each person’s unique experience.
“Virtually all these management guidelines start off with identifying who’s at risk and what patient- and disease-specific factors pose a higher versus a lower risk,” says Gary H. Lyman, a retired medical oncologist who was the co-director of the Hutchinson Institute for Cancer Outcomes Research and is a retired professor at the University of Washington in Seattle. “And of course, if there’s a higher risk of side effects, those are the patients you really want to focus the mitigation measures and supportive care measures [on].”
One of the biggest areas of improvement is in managing neutropenia, Lyman notes. This condition occurs when chemotherapy depletes neutrophils, white blood cells made in the bone marrow. A low white blood cell count compromises the body’s ability to fight off infection. If these counts fall dramatically, patients may develop a dangerous condition called febrile neutropenia, which can result in hospitalization and death. But oncologists now have better antibiotics to manage this condition.
Early in his career, Lyman says, “the biggest problem getting patients through treatment was many patients developed widespread infection and died from sepsis from bacterial and fungal infections. The advent of an increasing number of broad-spectrum antibiotics revolutionized the results for many of those patients early on.”
Patients who receive chemotherapy are typically counseled to call an oncologist if they develop a fever of 100.4 degrees or higher, which can be a sign of febrile neutropenia. Physicians routinely take blood samples between treatment cycles to make sure neutrophil counts are adequate. For patients at high risk of developing febrile neutropenia, oncologists prescribe drugs that can help the bone marrow produce more white blood cells to reduce the risk of developing the dangerous condition.
To minimize her risk of developing febrile neutropenia, Joergensen was sent home with Neulasta (pegfilgrastim) Onpro, a device that fits on the arm and injects a myeloid growth factor known as granulocyte colony-stimulating factor to help the bones produce neutrophils. Joergensen says the device was set to deliver medication 24 hours after she completed chemotherapy. “It’s really just so you don’t have to go back to the chemo center for another injection, but it just stimulates your white blood cell growth,” she says, noting the convenience but also the importance of avoiding interactions with others during the pandemic.
Patients with cancer are also at increased risk of developing blood clots called venous thromboembolisms—often resulting from the cancer itself but also related to cancer treatment in general as cancer cells break down in the blood. (To learn more, read “Preventing Blood Clots.”) Blood thinners called anticoagulants can treat blood clots and prevent them from developing in high-risk patients. Once administered only by injection, blood thinners can now be taken as pills, says Lyman.
Settling the Stomach
Nausea is likely to be one side effect that many patients fear when they learn they’ll be receiving chemotherapy. Typically not life-threatening, nausea is still bothersome for patients and a frequent cause for adjusting chemotherapy doses. Physicians can also prescribe antiemetic drugs that minimize vomiting and nausea.
“There are actually grades for how emetogenic different chemotherapy is,” says hematologist-oncologist Mikkael Sekeres of the drugs’ ability to cause nausea and vomiting. For some chemotherapies, patients are given prescriptions with instructions to use anti-nausea drugs if needed. For other chemotherapies, it’s not presented as optional, he says. “We give the nausea medicine because it is almost guaranteed someone’s going to get nauseated,” says Sekeres, chief of hematology and professor of medicine at the Sylvester Comprehensive Cancer Center at the University of Miami Health System.
Even though Joergensen was taking Adriamycin and Cytoxan, two drugs known to cause nausea, she did not vomit or feel sick to her stomach—likely because she was treated with drugs to manage the effects. Still, adding more drugs can lead to more danger for patients. For example, anticoagulants carry an increased risk for bleeding, so doctors prescribe them cautiously. Sekeres says he sometimes prescribes a chemotherapy drug called azacitidine for his patients with leukemia or myelodysplastic syndromes, which are a group of blood cancers. In past years, patients taking this drug would experience nausea and vomiting, but antiemetic drugs have eliminated the side effect. “I almost never hear a patient complaining of nausea [due] to this medicine, but I almost always have patients complain of constipation [due] to the nausea medicine,” Sekeres says. “So, I’ve traded one side effect for another hopefully much more bearable side effect. And now what we do is, we counsel patients about adequate hydration to avoid the constipation [due] to the nausea medicine.”
The Patient’s Role
With doctors able to manage many side effects, they encourage patients to speak up when treatments make them sick. “I think that patients hear they’re getting chemotherapy, and they assume, ‘OK, that means that I’m going to get nauseated and have diarrhea, and that’s all a normal part of chemotherapy,’” Sekeres says. “So when it happens, they may not contact the doctor’s office because they say, ‘Oh, this is what I was expecting would happen.’ But a take-home [for better side-effect management] is to contact the doctor’s office. Let us know you’re having those side effects so we can manage them.” Another reason patients are reluctant to share how sick their treatments are making them, Lyman and Kuderer say, is the fear of being taken off the regimen.
Joergensen says one of the hardest parts of her treatment was developing painful mouth sores—a condition known as chemotherapy-associated mucositis. She also experienced constipation, which she describes as the feeling of “passing shards of glass” when she had a bowel movement. She used magic mouthwash—an oral spray that includes several ingredients including a steroid, an antibiotic and a numbing agent—for her mouth sores. Given the severity of her symptoms, which could have been signs of an infection, she was also prescribed antibiotics, which pushed back her last chemotherapy treatment by a week and extended her countdown.
Maintaining a stable weight is a good goal to prevent treatment complications.
People who are about to start chemotherapy often have misconceptions about nutrition, says Joanna Lipp, an oncology dietitian at the University of Rochester Medical Center in New York.
“The majority of Americans are overweight, and they often think they could stand to lose a few pounds, but chemotherapy is a really bad diet regimen,” says Lipp, who has worked with cancer patients for 33 years. “It doesn’t end up giving you a beach body when you lose weight this way. All it does is make it harder for you to get through treatment.”
Chemotherapy dosing is based on body surface area, which is determined by a patient’s weight and height. “If your weight changes enough, treatments may need to be re-dosed or the treatment that you get may end up having more toxic effects,” she says. “Then, the treatment has to either be held or delayed. Every time treatment is altered like that, you decrease your chances of getting the most out of your treatment.” A better goal is to maintain or even gain weight, since many types of chemotherapy cause weight loss. That means choosing from a range of foods that patients can tolerate.
“You need enough calories to keep your weight stable,” Lipp says. Some patients can do that and get the nutrients they need in two meals per day, while others may need three meals and several small snacks. In some cases, patients may do better eating small amounts of food four to 10 times a day. She notes that people may experience taste changes, diarrhea and other side effects, which can alter the kinds of food they want to eat.
“Sometimes the foods they are used to eating don’t work very well, so we need to try to be open to working with some other foods,” Lipp says. She emphasizes adding healthy fats like avocados, nuts, nut butter and tahini.
While their goal for patients is to receive the recommended dosages of chemotherapy drugs, most oncologists understand the importance of adjusting chemotherapy dosage to ensure patients can continue treatment. “We try to manage the side effects as best we can, but when they’re not adequate to the patient experience, we will work with the patient and we will reduce the doses,” says Lyman. He notes that this represents a shift in thinking for oncologists, many of whom were adamant about delivering the recommended regimens no matter what. Adhering to recommended doses is important, Lyman says, but not if it means patients get so sick that they can’t continue. “We have learned to be more flexible or bendable based on those ongoing, continuing discussions with patients about what they’re experiencing,” he says.
Kuderer notes that newer cancer treatments, often combined with chemotherapy, make it more difficult for oncologists to discuss all relevant side effects from each treatment regimen. She stresses that patients should talk with their doctors about the potential impact of treatment on their favorite activities and their livelihood. She points out that mental fog—also called chemo brain—can impact job security for cancer survivors whose jobs require mental exertion, while physical effects from chemotherapy, such as numbness in feet and hands called neuropathy, can affect workers with jobs that require strength and dexterity.
When patients are considering the risks and benefits of different treatments, Kuderer recommends they give doctors permission to be candid with them. She suggests putting a simple question to the doctor: What would they advise if a loved one was in the same situation? “It’s a beautiful question. It gets to that personal level,” she says. “It ensures that the clinician in front of you sees you really as a human being and that unique individual that you are, and it brings them in that mindset.”
Joergensen is grateful for an ongoing dialogue with her oncologist. Her initial treatment ended with 28 rounds of radiation. In August 2022, she started on Verzenio (abemaciclib), a targeted treatment known as a CDK4/6 inhibitor, to reduce her chances of a recurrence.
For someone who prides herself on seeing the bright side, Joergensen has had more than her share of sadness over the past few years. Her sister died of inflammatory breast cancer in 2019, seven months before Joergensen received her own breast cancer diagnosis. Her mother entered hospice in Denmark in February 2024 after being diagnosed with triple-negative breast cancer in 2021. Still, Joergensen finds strength in having made it this far. She looks back to her first days of treatment in 2020, being dropped off at the hospital at 6 a.m. for surgery to remove both her breasts. She felt alone and filled with uncertainty.
“I stood there with my suitcase, just [thinking], ‘Is this for real?’ because it felt so unreal,” she says. “But that’s another thing: You can do more than you think you’re capable of, and you realize that when you go through things like chemo. We are a lot more resilient than we give ourselves credit for.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.