When Kevin Lewis’ daughter, Katie, was born in 2007, he fell in love all over again. And like new parents everywhere, he couldn’t help but wonder how her life would unfold, what interests they would share, which family traditions she would choose to carry on. But Lewis also had a deeper concern: Had Katie inherited the genetic mutation he carried that would greatly increase her risk of developing cancer?
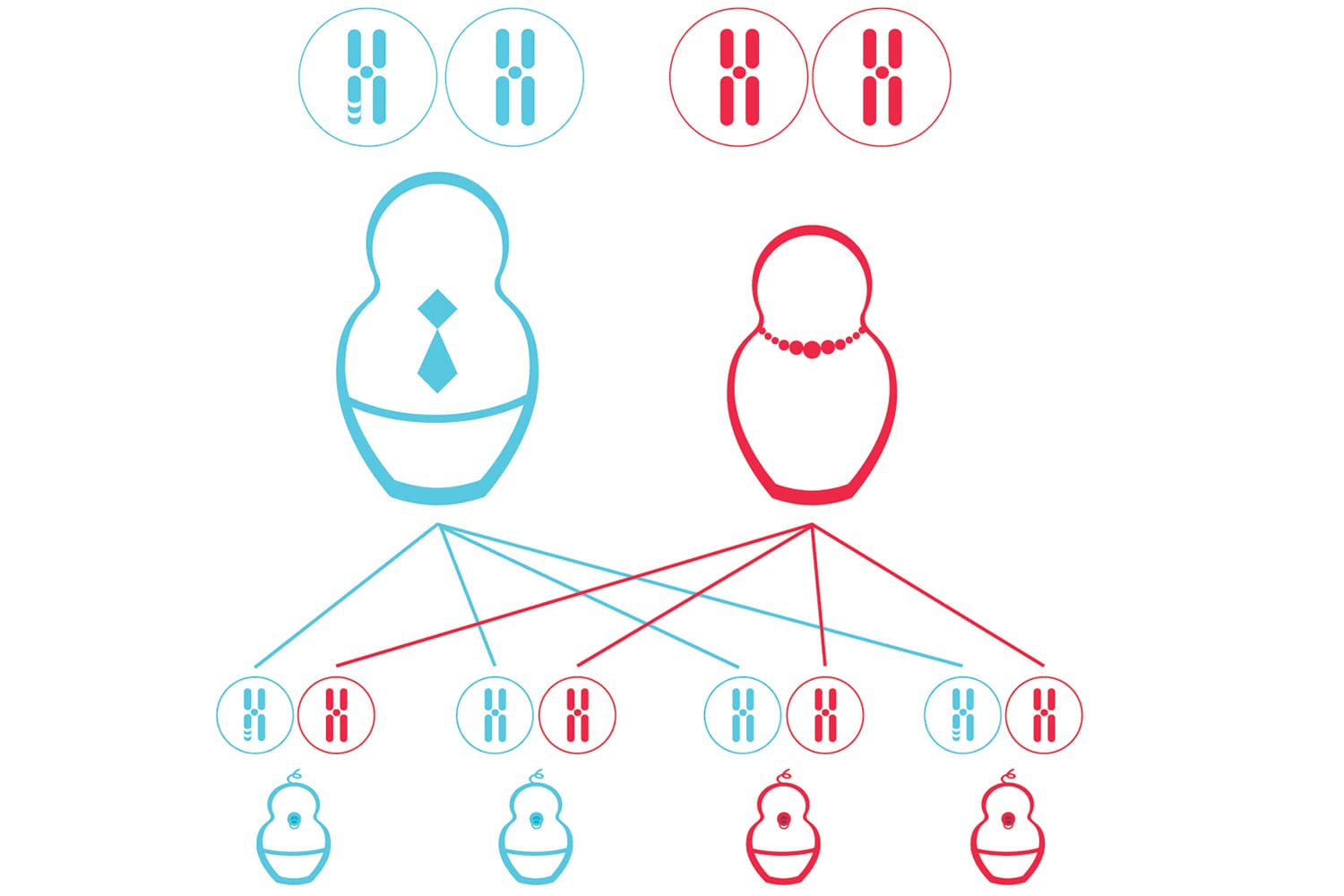
About 5 to 10 percent of all cancer cases can be traced to an inherited mutation. Determining a more precise figure is difficult because many people are not aware of their family’s health history and not all people who are told they might carry a mutation choose to be tested. Those like Lewis who find out their status often face difficult decisions and ethical crossroads: how to tell family members and whether to test a child. Another consideration is whether to take advantage of reproductive technologies that can virtually ensure their child will not face the same choices.
Family Ties
Lewis, a management consultant from South Woodstock, Conn., learned that a genetic mutation was fluttering through his family tree after his cousin was diagnosed with colorectal cancer in 1997. Because of his young age—early 40s—and a family history of cancer, doctors suggested that the cousin be tested for a mutation in the MSH2 gene, which had recently been linked to a hereditary condition known as Lynch syndrome. A person diagnosed with Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), has an 80 percent lifetime chance of developing colorectal cancer. Those with the syndrome also have an increased risk of cancers of the stomach, small intestine, liver, gallbladder ducts, upper urinary tract, brain and skin, as well as uterine and ovarian or prostate cancer.
When his cousin tested positive for Lynch syndrome, Lewis, then 33, was invited to take part in a clinical trial that was investigating how families respond to genetic testing. “They walked my cousin through our family tree, starting with the assumption that his father was positive because of his bouts of cancer,” Lewis says. “That led them to test my dad, who had had colon cancer twice, and he was positive. And then my brothers and I were tested, too.” Like Lewis, one of his brothers also tested positive.
The results of the genetic test immediately changed Lewis’ medical care. “I had been having a colonoscopy every three to five years because my dad had colorectal cancer,” he says. “That went down to annual. … I also had to begin having a biannual skin exam because Lynch syndrome is also associated with Muir Torre,” a skin cancer syndrome that increases the risk of four rare types of skin tumors: sebaceous adenomas, sebaceous carcinomas, sebaceous epitheliomas and keratoacanthomas.
Lewis, now 48, would not have had the opportunity to take advantage of this early screening if his cousin’s doctors hadn’t been well informed. “Most primary care physicians do not go over the family history in depth,” notes Rizwan Hamid, a cancer geneticist at Vanderbilt University Medical Center in Nashville, Tenn., “and somewhat surprisingly, many oncologists are also so busy” they don’t do it either.
Many doctors also ask the wrong questions. Because most hereditary cancer syndromes involve many types of cancer, asking a patient if other family members have had the same type of cancer is not as good as asking whether anyone in the family has had any cancer, Hamid explains. And then, red flags for inherited cancers may be missed.
When to Test
Learning that a relative has cancer may make some people want to run out and get tested for genetic mutations that increase cancer risk. But the first step, geneticists stress, should be to talk with a genetic counselor, who can explore the family tree and explain what testing can (and can’t) do.
“The goal of testing,” explains Rebecca Nagy, a genetic counselor at Ohio State University, in Columbus, is not to just acquire information, “but to prevent healthy individuals from ever getting cancer in the first place.” It makes sense then, she says, that the person who has been diagnosed with cancer is typically first to be tested; if that individual doesn’t have a mutation, there is no reason to consider testing his or her children. Likewise, testing should not be done until a person has reached an age at which the cancer risk associated with the mutation can be reduced through screening, surgical procedures or lifestyle change.
Understanding this reasoning, genetic counselors stress, is especially important for parents of young children. “As geneticists, we are much more shy about doing testing in children than [in] other people,” says Hamid. “The typical approach that most geneticists use is if there is no intervention that can be done for a child, then there is no point in doing testing.”
For instance, a child who has a mutation in the RET gene that causes a rare inherited cancer syndrome called multiple endocrine neoplasia type 2A (MEN2A) has a 98 to 100 percent chance of developing medullary thyroid cancer, Hamid says. “If I saw a child who had a parent with MEN2A—not MEN2B—we’d test that child early, because if they test positive, they may be a candidate for very early removal of their thyroid gland. Testing as early as age 6, 7 or 8 is appropriate. And that’s because we can decide on management based on the answer we get—there is something that can happen” if the test result is positive.
For other genetic mutations, like BRCA1 and BRCA2, which increase the risk of breast, ovarian and prostate cancers, genetic counselors do not recommend testing until adulthood, when risk-reduction options, like screening or surgery, could be introduced. Niecee Singer Schonberger, a genetic counselor at Sharsheret, an organization that provides breast cancer information and support to Jewish women, has had many conversations with women about how and when to talk to their kids about testing.
“There are some women who tell me that they will not discuss the BRCA mutation with their children until later,” she says. “And there are others who say they are open with their children, especially if they are older teens, or girls. Sometimes a woman will say, ‘I want to test my 16-year-old,’ but that’s not recommended, and the lab probably wouldn’t do it.”
That’s because risk reduction guidelines for women who carry a BRCA mutation suggest breast cancer screening should begin only when they reach their 20s. “There’s nothing a child can do,” says Schonberger, who believes the genetic test results would just create anxiety. It’s often a mother who wants to know, she notes, “and so I explain that this is the child’s life and the child’s decision to make as an adult. She may not want the test, or she may want to wait, or she may not be ready for the information. It’s their child, but it’s their child’s genetic information.”
The Next Generation
Advances in reproductive technologies have opened up a new opportunity—and ethical questions—for individuals carrying a genetic mutation: using in vitro fertilization (IVF) techniques along with preimplantation genetic diagnosis (PGD) to select and use only embryos that have been determined to not carry a genetic mutation.
Genetic counselors say they are just starting to see patients with an inherited cancer mutation consider this option. It is much more commonly used, they say, by people with a genetic mutation that will cause an illness affecting a child from birth, such as Tay-Sachs disease or sickle cell anemia. And there is a distinction, they explain, between passing on a mutation that causes a disease and passing on a cancer mutation that increases the risk of getting a disease—and for which there are screening programs in place that can help mitigate that risk.
“When people ask about prenatal diagnosis, I tell them about IVF and PGD,” says Schonberger, “but when you think about it, what you are doing is taking a couple who is presumably fertile and having her go through uncomfortable procedures that involve taking hormones, and that are very expensive … [and you are] talking about an embryo who will develop into a child … who might not develop any cancer for 40 or 50 years, and in 40 or 50 years the whole scenario is going to be very different”—there may be earlier treatment options, there may be cures.
“I think a lot of how a woman will react to this information is determined by how much suffering she has seen in her family,” she adds. “If she had a sister or mother who suffered terribly, she is going to react differently than someone who has not had that history.”
Anna, a 23-year-old single woman living in the San Francisco Bay Area, is taking actions that could ensure she will be the end of the line for her family’s inherited cancer genes. (Anna requested that her last name not be used because she did not want her decisions to affect her career.) Her grandmother was diagnosed with ovarian cancer at age 61, in March 2007, and died nine months later. Knowing that her grandmother’s grandmother had had breast cancer and that her grandmother’s mother may have had an abdominal cancer made Anna, then 18, and her mother think that their female relatives harbored a genetic mutation. As a first step, Anna’s grandmother was tested for the BRCA mutation a few weeks before she died: The result was positive. Shortly after Anna’s grandmother was tested, Anna’s mom learned she had the mutation. And when Anna turned 21, she found out she had it, too.
“I kind of knew that I wanted to be tested early,” she says. “I spoke with a few family friends who were physicians and my mother’s gynecologist and they all said, ‘We don’t recommend testing until 25, for emotional and psychological reasons … and because it’s not recommended that women start mammography screening until then—so why worry?’ For some people that’s good advice. But I wanted to know if I was at increased risk of developing breast and ovarian cancer, because knowing meant I could take action and do something about it.”
In the same vein, when her genetic counselor told her that it was possible to use reproductive technologies to freeze her eggs (a process called cryopreservation), Anna decided to begin exploring that option. Earlier this year, after an exam showed a low egg count for someone her age, Anna underwent two cycles of ovarian stimulation, which allowed her to freeze about 60 mature eggs.
Initially, she says, she thought of the eggs as something she’d have in reserve, just in case she had to have her ovaries removed because she developed ovarian cancer or they became damaged during breast cancer treatments. Then, she began to think about what PGD could offer: the ability to test her eggs after they are fertilized and only implant those embryos that don’t carry the mutation. Now, she is considering using it when she is ready to become pregnant. “I don’t want my kid to have to go through” this, she says. “And I don’t want to pass on the mutation. … But I also know this isn’t right for everyone.”
Lewis and his wife are two of those people. Around the time they were trying to conceive, PGD was being introduced into the cancer arena. But it was never an option they seriously considered. “We casually talked about it,” he says, “but I had been on a lot of panels at medical conferences with folks with other genetic disorders [and I felt that] for some of the other genetic conditions it makes more sense” than it does for Lynch syndrome.
Katie, who is now 5, hasn’t yet been tested for Lynch syndrome, because children who carry Lewis’ mutation typically don’t have their first colonoscopy until their 20s. However, given Katie’s possible increased risk for skin cancers, Lewis says, he and his wife are already conscientious about limiting her sun exposure.
But as he said one evening in June while building a bookcase for his daughter, he couldn’t be more optimistic about her future, citing the measures available to prevent some Lynch syndrome cancers—such as colonoscopy, which can detect and remove colorectal polyps before they turn cancerous—and his belief that other related cancers will be easily detectable, or perhaps even preventable, in Katie’s lifetime. “Maybe I have a bad gene,” says Lewis, “but there are far worse things to have than Lynch syndrome.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.