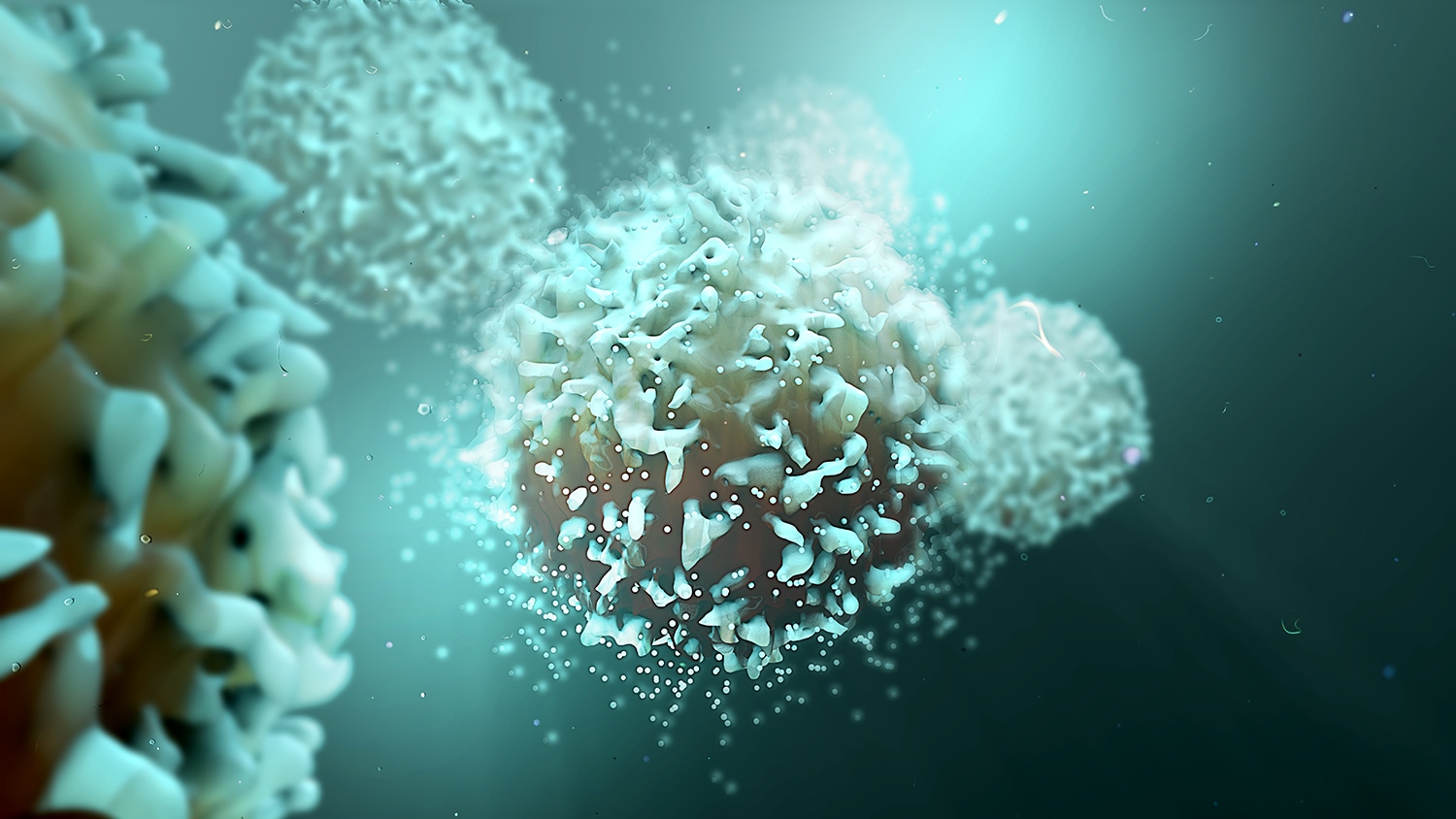
Exploring Immunotherapy Side Effects
Researchers have reviewed 125 clinical trials of immunotherapy drugs, finding that around two-thirds of patients experience side effects from the drugs. The study, published April 25 in JAMA Oncology, looked specifically at trials of immune checkpoint inhibitors targeting the proteins PD-1 or PD-L1. The most common side effects were fatigue, itchy skin and diarrhea. Adverse events grade 3 (considered severe) or higher were reported in 14% of patients. Out of 18,353 patients in trials that reported whether treatment-related deaths occurred, 82 patients died of adverse events related to checkpoint inhibitors. Meanwhile, a second JAMA Oncology study published the same day looked at whether side effects were associated with treatment response in patients with non-small cell lung cancer. Of 73 patients on checkpoint inhibitors, 25 had immune-related skin reactions. Patients who had complete or partial responses to therapy were more likely to have these side effects. The researchers also analyzed immune cells called T cells found in the skin lesions and lungs of these patients. T cells attack when they recognize specific molecules, called antigens, on other cells. The researchers found the T cells in the patients who responded to therapy were recognizing the same antigens in both the skin and the lungs.
Prior Authorization: An Obstacle to Care?
Insurers require that doctors get prior authorization before giving certain treatments, including some drugs, surgeries and radiation. A survey of radiation oncologists indicates that many view this requirement as a burden. The American Society for Radiation Oncology (ASTRO) sent the survey out to its members, getting 673 responses. They found that 93% of these radiation oncologists believed that prior authorization delayed their ability to give patients life-saving treatments. Nearly one-third said that delays lasted more than five days on average. The physicians also said that the prior authorization gave them extra work; 63% of respondents said they or their practice had brought on additional staff in the last year to deal with prior authorizations. A previous ASTRO survey showed that radiation oncologists viewed prior authorization as the No. 1 challenge facing the field. “Radiation oncologists increasingly are restricted from exercising our clinical judgment in what is in the best interest of the patient, yet we are held accountable for the outcomes of treatments where decisions have been taken out of our hands,” Vivek Kavadi, vice chair of ASTRO’s Payer Relations Subcommittee and a radiation oncologist at Texas Oncology, said in a press release.
Another Immunotherapy Approval
The U.S. Food and Drug Administration on April 19 issued another approval for Keytruda (pembrolizumab), an immune checkpoint inhibitor. Keytruda combined with the targeted therapy Inlyta (axitinib) is now approved for patients with advanced kidney cancer. Previously, Inlyta given alone was approved for kidney cancer. Other checkpoint inhibitors have also been approved for treating advanced kidney cancer in the past.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.