Every week, the editors of Cancer Today magazine bring you the top news for cancer patients from around the internet. Stay up to date with the latest in cancer research and care by subscribing to our e-newsletter.
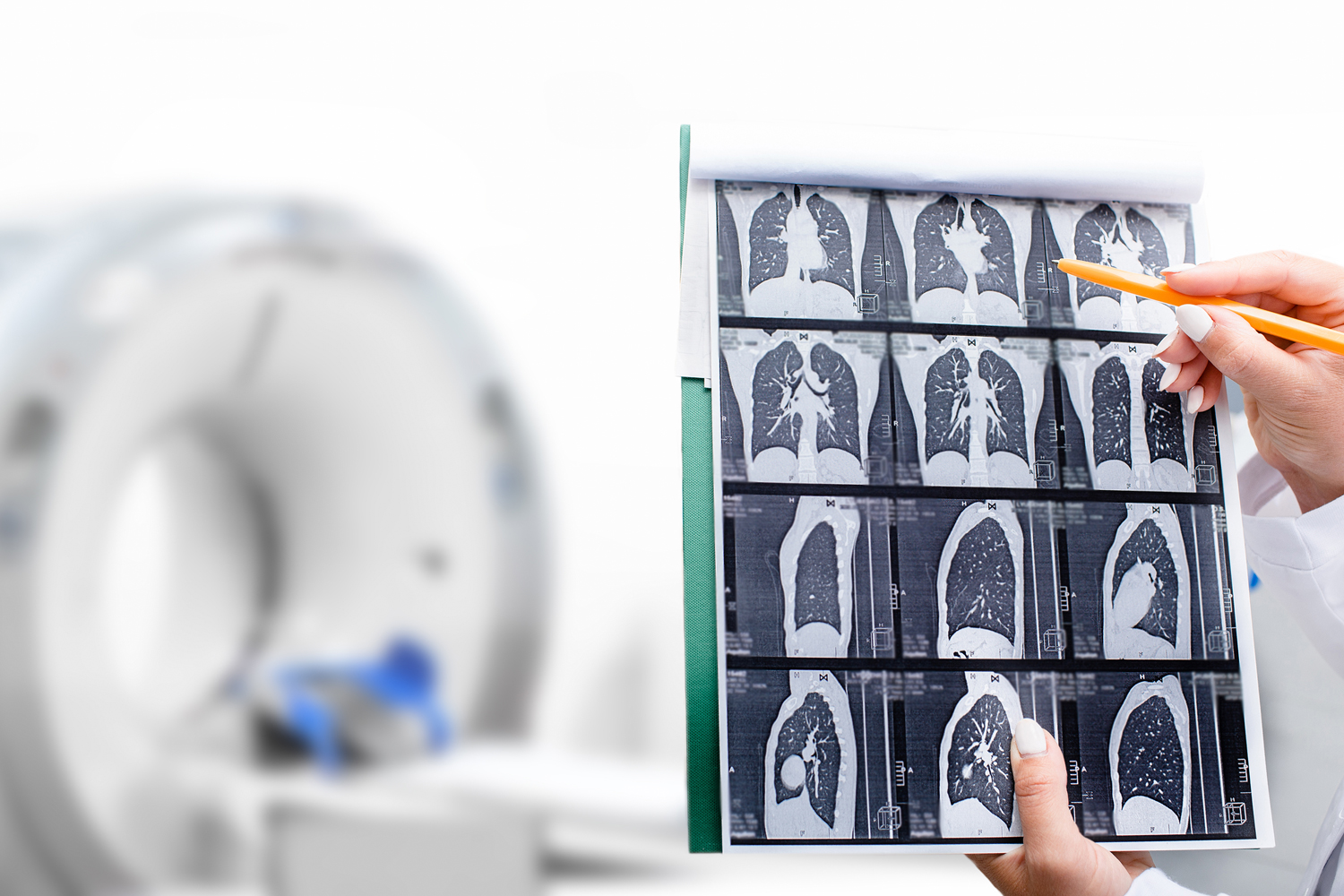
1 in 5 Eligible People Underwent Lung Cancer Screening in 2024
Since March 2021, the U.S. Preventive Services Task Force has recommended that adults ages 50 to 80 with a significant smoking history have an annual CT scan to screen for lung cancer. The recommendation applies to those with a 20 pack-year smoking history who either currently smoke or quit within the last 15 years. People with a 20 pack-year smoking history have smoked at least two packs of cigarettes a day for 10 years or an equivalent amount, the New York Times reported. However, people have been slow to comply with the recommendations, as 1 in 5 people who qualified underwent lung cancer screening in 2024, according to a research letter published in JAMA. Researchers reviewed survey responses from 2,124 people eligible for lung cancer screening based on the 2021 recommendations. Nearly 19% of screening-eligible people reported being up to date on their lung cancer screening. Rates were lower in people younger than 60 and higher in those with other conditions, like heart disease or asthma. If rates increased to 100% in eligible people, the researchers projected screening could prevent over 62,000 deaths over a five-year period, MedPage Today reported. Additionally, everyone whose life was spared would live approximately 14 years longer, according to the Times. The study also included an additional 4,390 screening-ineligible people, of whom 18.1% had a smoking history of at least 20 pack-years but quit more than 15 years earlier. For people ineligible for lung cancer screening, 100% uptake could prevent over 29,000 deaths. The findings may warrant revisiting current eligibility recommendations for lung cancer screening, the researchers wrote. “Each year, many individuals die of lung cancer who probably would still be alive had they been screened—reflecting both low uptake among currently eligible adults and overly restrictive eligibility criteria that exclude many at high risk,” Chi-Fu Jeffrey Yang, a thoracic surgeon at Massachusetts General Hospital in Boston, and colleagues wrote in an accompanying editorial.
Breast Cancer Risks Depends on the Type of Birth Control
The amount of progestin, a substance resembling the female hormone progesterone, may be the driver in which types of birth control increase breast cancer risk more than others, a study published in JAMA Oncology found. Researchers analyzed data from over 2 million adolescent girls and women, approximately 16,300 of whom were diagnosed with breast cancer during an average of 10 years’ follow-up. Women who had ever used hormonal birth control had a 24% higher risk for developing breast cancer than those who had never used it. In other words, out of every 7,752 women who have used birth control, one of them will be diagnosed with breast cancer. However, researchers noticed results varied when broken down by birth control type. Taking birth control containing estrogen and progestin increased a woman’s breast cancer risk by 12%, whereas using birth control with progestin alone increased it by 21%. Oral birth control containing desogestrel, a synthetic hormone that acts like progesterone, either alone or in a combination increased the risk for breast cancer by 18% to 19%. Implants with etonogestrel, a synthetic hormone typically inserted in a person’s arm, increased a woman’s breast cancer risk by 22%, compared with 9% for oral pills containing a combination including the synthetic hormone levonorgestrel. A hormonal intrauterine device with levonorgestrel increased this risk by 13%. Of note, researchers saw no significant increased risk with the etonogestrel vaginal ring, medroxyprogesterone acetate injection or oral pills containing drospirenone, a synthetic type of progestin, although many women in the study used these formulations. Despite these findings, posts on TikTok and other social media platforms have assumed the results mean that all birth control causes cancer, highlighting how study findings can easily be taken out of context, KFF Health News reported. “I get really angry at this because it’s designed to scare people like me away from birth control, which has made my life so much better in many ways,” Rachel Fey, interim co-CEO of Power to Decide, an organization that advocates for the right to choose whether to get pregnant and have a child, told KFF Health News. “It’s really frustrating … especially when it’s given without context. And then in this era of social media, it can just take off without anybody who knows what they’re talking about providing that context.”
Immunotherapy Side Effects Can Increase Risk for Colon Adenoma
People who received immune checkpoint inhibitors to treat cancer and developed diarrhea and colitis—known side effects of the drugs—have an increased risk for adenomas in the colon, according to research presented at the American College of Gastroenterology 2025 Annual Scientific Meeting in Phoenix. Adenomas, a type of colon polyp, form as non-cancerous tumors in gland-like cells of tissues that line organs and other parts of the body. Because adenomas are the polyps that most often change into colorectal cancer, health care professionals recommend removing them to prevent them from growing larger or becoming cancerous. “The cancer population is already at a higher baseline adenoma risk, and our findings show that [immune checkpoint inhibitor]-mediated diarrhea and colitis compounds this,” Tanvi Gupta, a study author and the chief medical resident at the University of Texas Health Science Center in Houston, said during the presentation. Immune checkpoint inhibitors, like PD-1 and PD-L1 inhibitors, have proven to be effective treatments for many cancers. However, since immune checkpoint inhibitors take the brakes off of the immune system so it can recognize and attack cancer cells, they can also cause chronic inflammation, leading to side effects such as diarrhea and colitis, which is inflammation of the colon. In the study, researchers analyzed data from 248 people who developed diarrhea and colitis from immune checkpoint inhibitors, as confirmed by colonoscopy. Most people in the study had melanoma or a genitourinary cancer, like kidney, bladder or prostate cancer. Of the people in the study, 71 developed adenomas, with over 50% of the polyps developing within 7.5 months of the start of diarrhea and colitis symptoms, Medscape reported. The rate at which adenomas developed declined over the following six years. In 210 people who underwent follow-up colonoscopy within one year of experiencing diarrhea and colitis, nearly 16% of those without a history of polyps developed adenomas, compared with nearly 34% of people who had a history of polyps. Despite having no prior history of polyps, people who developed these side effects had a higher risk for developing adenomas than those who didn’t. Additionally, people with a history of inflammation and adenomas when starting treatment with immune checkpoint inhibitors were significantly more likely to develop new adenomas.
Editor’s Note: The Week in Cancer News will not be published Nov. 28 due to the Thanksgiving holiday. The next Week in Cancer News will be posted Dec. 5.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.