Every week, the editors of Cancer Today magazine bring you the top news for cancer patients from around the internet. Stay up to date with the latest cancer research and care by subscribing to our e-newsletter.
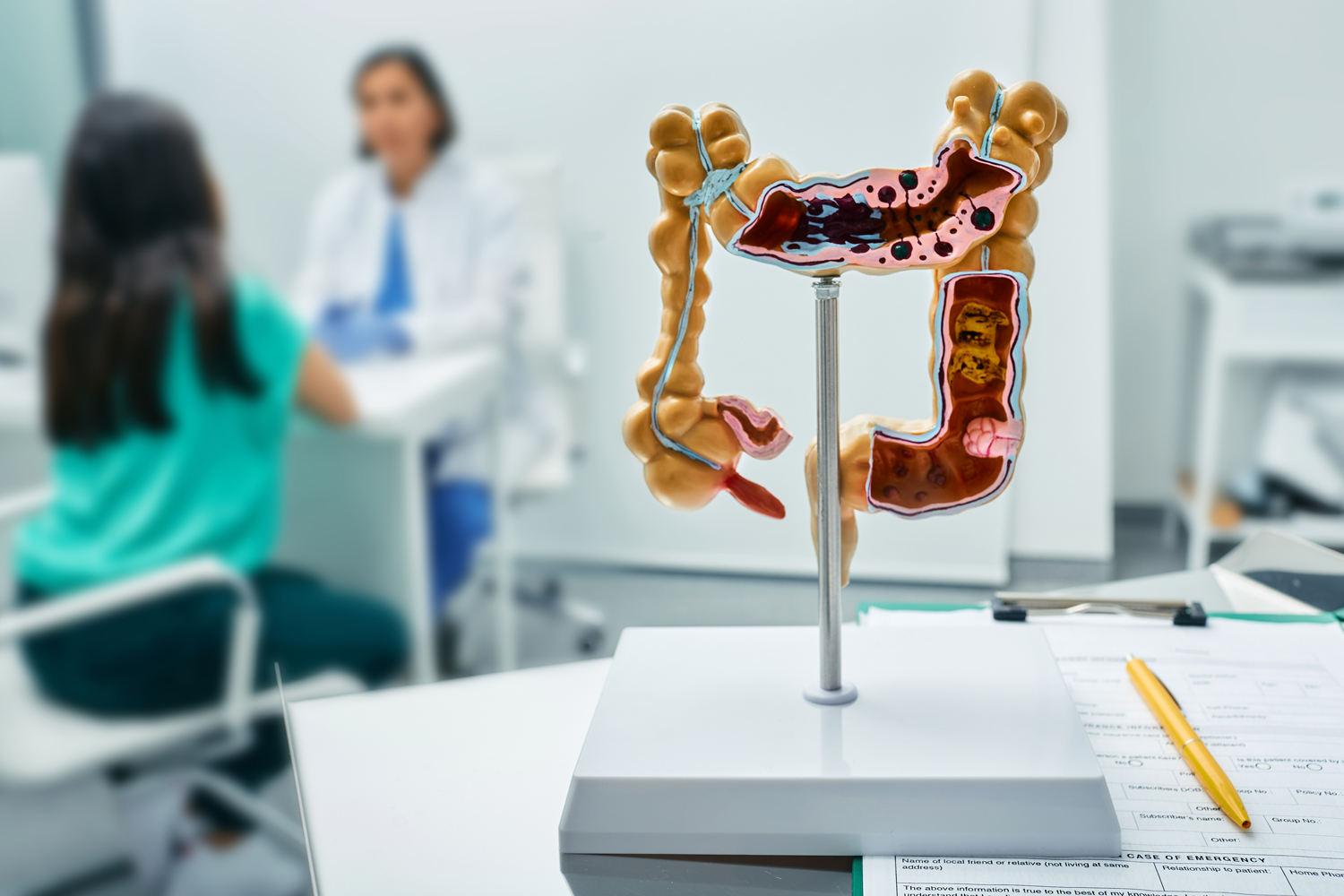
Many With History of Polyps Skip Follow-Up After At-home Screening
Screening guidelines advise that people who have any polyps removed during a colonoscopy continue screening with colonoscopies in the future. Although guidelines don’t go so far as to recommend screening with newer stool-based tests, such as at-home fecal immunochemical test (FIT), many people use at-home tests to detect signs of colorectal cancer. To examine screening habits after colonoscopy and the use of FIT, researchers reviewed medical records from the Veterans Health Administration for 4.8 million people who got a colonoscopy between 2000 and 2024, Medscape reported. The study, presented at the 2025 American College of Gastroenterology (ACG) Annual Scientific Meeting, showed that about 11% of people used FIT within 10 years of their colonoscopy, nearly half of whom had polyps removed at their initial colonoscopy. Only 50.4% of people who had polyps removed on a colonoscopy and had a subsequent positive FIT result followed up with a colonoscopy suggesting that even those who have higher risk of developing colorectal cancer do not follow up to receive a colonoscopy, which can both find and remove polyps. Among people who had a previous colonoscopy that did not remove any polyps, the rate of follow-up after a positive FIT result was 49.3%. “The main message that needs to get out to people who are undergoing stool-based screening is that the stool test is only the first part of the screening process, and if it’s positive, a follow-up colonoscopy must be performed. Otherwise, the stool-based test is of no value,” William D. Chey, a gastroenterologist at University of Michigan Health in Ann Arbor, said in Medscape.
Early-onset Cancer Rate Rises in Corn Belt
Young adults in states that make up the nation’s Corn Belt—Iowa, Kansas, Illinois, Minnesota, Indiana and Nebraska—are getting cancer at rates that are rising faster than in the rest of the country, according to a report in the Washington Post. In 1999, cancer diagnoses in these six states were in line with the rest of the country. But, according to an analysis by the Post, their trajectory began to diverge soon after. By 2022, the region’s rate of cancer in young adults was 5% higher than the national average for young adults. Around 2000, Iowa ranked 18th among U.S. states for cancer in adults under 50. Today, it ranks fifth. “What’s driving these rates is what is on everyone’s mind, including mine, all the time,” said Mary Charlton, an epidemiologist and the director of the Iowa Cancer Registry, in the Post. “The complicated thing is that it’s not risk factors now. It’s our risk factors from 10, 20, 30 years ago that are causing the cancers now.” Known risk factors include elevated UV light exposure from outside work and high rates of binge drinking. But researchers are investigating other potential exposures that could increase risk, such as radon levels, nitrate pollution in groundwater from fertilizer use, and chemicals used to kill pests and weeds in commercial farming operations.
Bispecific Antibody Improves Cancer Control in Advanced Non-small Cell Lung Cancer
A bispecific antibody given with chemotherapy extended how long some people with advanced squamous non-small cell lung cancer (NSCLC) lived without their cancer progressing, according to clinical trial results presented at the European Society for Medical Oncology (ESMO) Congress 2025 last week in Berlin. According to the findings, which were also published in the Lancet, people who received chemotherapy plus ivonescimab, a bispecific antibody that targets two proteins in cancer cells, lived about 11 months without cancer progression, while those who received an immune checkpoint inhibitor, called Tevimbra (tislelizumab) plus chemotherapy lived nearly 7 months without disease progression, Oncology News Central reported. People given ivonescimab and chemotherapy had more higher-grade side effects that required medical attention, which were seen in 63.9% of people given ivonescimab and 54.3% of people given Tevimbra. While presenting the findings at ESMO Congress 2025, Shun Lu, the chief of Shanghai Lung Cancer Center at the Shanghai Chest Hospital in China, said the study could lead to a new standard of care. An invited discussant for the study, Myung-Ju Ahn, a hematologist-oncologist at Samsung Medical Center in Seoul, South Korea, noted the findings raised the bar, but cautioned that it is still too early to know if the bispecific antibody can help people live longer. “It represents an important first step and a new benchmark in the management of squamous non-small cell lung cancer, but we have several unanswered questions,” Ahn said, in the Oncology News Central report.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.