Uncharted Territory
When Gene Bishop was diagnosed with Hodgkin lymphoma at age 18 in 1965, researchers had recently discovered that radiation for the cancer could lead to long-term survival. But the therapy that cured her cancer went on to cause heart problems, breast cancer and thyroid cancer, she writes in an essay in the Journal of Clinical Oncology. Now Bishop, who is a physician herself, has stage IV non-small cell lung cancer, also likely a result of her Hodgkin lymphoma treatment. It is likely to kill her. “Both my oncologist and I are living with the reminder that no treatment does only what we want it to do and that one year’s miracles may have serious consequences even 50 years later,” she writes. “And although some of these may be known, or theoretically possible, many are not even imagined until one, two, three or many case reports begin to appear and random events turn into warnings and known consequences.”
More Treatment Isn’t Necessarily Better
Patients with locally advanced uterine cancer fare similarly whether they receive a combination of chemotherapy and radiation after surgery or just chemotherapy after surgery, according to results of a phase III trial published June 13 in the New England Journal of Medicine. The researchers estimated that five years after treatment, 59% of patients who received both chemotherapy and radiation and 58% of those who received just chemotherapy would be alive and free of recurrence. At one time, standard therapy for these patients was radiation therapy alone. Nearly 15 years ago, a trial comparing chemotherapy and radiation showed that chemotherapy was superior. Today, many patients receive both radiation and chemotherapy, but the new study indicates that this is not necessary. “In general, in cancer care, if you can get the same result by using one therapy, there is no reason to use two,” Kevin Holcomb of Weill Cornell Medical College in New York City, who was not involved in the study, told Medscape Medical News.
New Immunotherapy Indications
The U.S. Food and Drug Administration (FDA) on June 10 approved the immune checkpoint inhibitor Keytruda (pembrolizumab) for initial treatment of head and neck cancer patients whose cancer is metastatic or has returned and cannot be removed surgically. Patients whose tumors express the protein PD-L1 can take Keytruda on its own. Others can take Keytruda combined with chemotherapy. Immunotherapy drugs have previously been approved for treatment of patients with advanced head cancer who have already tried chemotherapy.
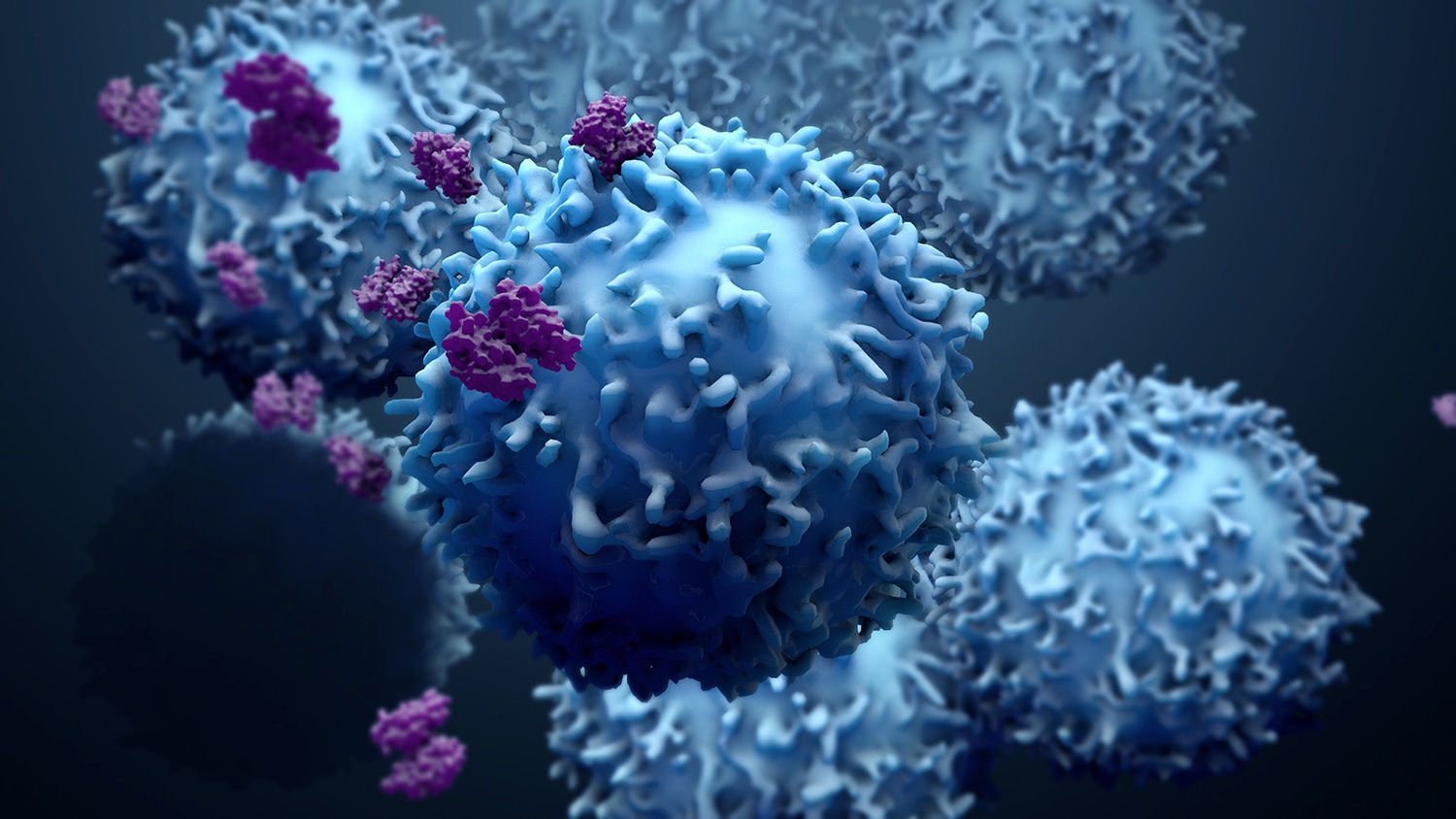
A Targeted Therapy for Lymphoma
Some molecules are so toxic to cells that they cannot be given on their own as chemotherapy drugs. Antibody-drug conjugates are drugs made up of a drug attached to an antibody that targets specific cells, delivering the drug in a targeted fashion. On June 10, the FDA approved a new antibody-drug conjugate for treatment of patients with relapsed or refractory diffuse large B-cell lymphoma who have already tried two other therapies. Polivy (polatuzumab vedotin-piiq) is composed of an antibody that targets B cells linked to MMAE, a drug that is toxic to cells. Polivy is approved when given alongside another chemotherapy drug and rituximab or a biosimilar product.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.